More Information
Submitted: March 04, 2024 | Approved: April 08, 2024 | Published: April 09, 2024
How to cite this article: George B, Mathai S, Shaji AM, Abraham CE, Johnson J. Proportion of Risk of Stroke among Male Patients Attending Outpatient Department of a Tertiary Care Hospital, Ernakulam District, Kerala. Clin J Nurs Care Pract. 2024; 8: 031-035.
DOI: 10.29328/journal.cjncp.1001054
Copyright License: © 2024 George B, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Proportion of stroke risk; Stroke risk score card; Patients
Proportion of Risk of Stroke among Male Patients Attending Outpatient Department of a Tertiary Care Hospital, Ernakulam District, Kerala
Betcy George1*, Susan Mathai2, Ansha Mol Shaji2, Christy Elsa Abraham2 and Jisna Johnson2
1Assistant Professor, Department of Medical-Surgical Nursing, MOSC College of Nursing, Kolenchery, Ernakulam, Kerala, India
2III year B.Sc Nursing Students, Kerala, India
*Address for Correspondence: Ms. Betcy George, Assistant Professor, Department of Medical-Surgical Nursing, MOSC College of Nursing, Kolenchery, Ernakulam, Kerala, India, Email: [email protected]
Aim: A descriptive-analytical study was done to assess the proportion of the risk of stroke among male patients attending the outpatient department of a tertiary care hospital, in Ernakulam District, Kerala.
Objectives: The objectives of the study were to assess the proportion of the risk of stroke among male patients attending outpatient departments and to determine the association of stroke risk level with socio-personal variables.
Methods: The research approach of the study is a quantitative approach. The research design selected for the study is a descriptive-analytical design. The convenience sampling method was used for sample selection. The study was done in MOSC Medical College Hospital, Kolenchery among 288 male patients who met the inclusion criteria. Data collection was done using socio-personal proforma and stroke risk scorecards.
Results: Collected data were analysed by using descriptive and inferential statistics presented in tables and pie diagrams. The study findings revealed that out of 288 subjects, 43.4% have low stroke risk, 13.9% are in caution and 42.7% have high stroke risk. The findings also revealed that there is a significant association of stroke risk level with age, education, occupation, BMI and place of residence.
Statement of the problem: Proportion of risk of stroke among male patients attending outpatient department of a tertiary care hospital, Ernakulam district, Kerala. Proportion of risk of stroke among male patients attending outpatient department of a tertiary care hospital, Ernakulam district, Kerala.
Stroke represents an enormous public health burden. The terms brain attack and cerebrovascular accident (CVA) are also used to describe stroke [1]. Stroke is an umbrella term that refers to a functional abnormality of the central nervous system that occurs when the blood supply to the brain is disrupted. The universal symbol of stroke is a lightning bolt. There are lightning strikes in the form of strokes happening around the world at least once per minute. Millions of people have suffered from this disability worldwide [2].
The most important modifiable risk factors for stroke are high blood pressure and atrial fibrillation Other modifiable risk factors include high blood cholesterol levels, diabetes mellitus, cigarette smoking, heavy alcohol use, drug use, lack of physical activity, and obesity. Smoking just one cigarette per day increases the risk by more than 30%. Alcohol use could predispose to ischemic stroke and intracerebral and subarachnoid haemorrhage [2].
The World Health Organization (WHO) defines stroke as a rapidly developing clinical sign of focal (global) disturbance of cerebral function, lasting more than 24 hours or leading to death, with no apparent causes other than vascular origin [1].
Globally in the year 2015 stroke was the second most frequent cause of death in the world. 15 million people develop stroke each year [3]. Of these 5 million die and another 5 million are permanently disabled and high blood pressure contributes to 12.7 million strokes worldwide. By 2020 the annual number of deaths from stroke is projected to increase in men and the global death is projected to rise 7.8 million in 2030 [4].
In the 20th century, a major risk factor for stroke was identified and their relative impact is estimated. Globally, 51% of stroke deaths are attributable to high systolic BP and local rates of incidence of stroke are correlated with the prevalence of hypertension. Hypertension is the number one risk factor and a major determinant of both ischemic and haemorrhagic stroke [5].
Men’s stroke incidence rates are 1.25 times greater than women’s. The current male/female incidence was 1.59 for ages 65–69; 1.46 for ages 70–74; 1.35 for ages 75–79 and 0.74 for age 80 and older [2].
The stroke risk scorecard developed by the National Stroke Association contains risk factors and is divided into 3 categories, high risk, caution, and low risk denoted with red, yellow, and green colour respectively. A scorecard provides an idea of a person's stroke risk. This scorecard is widely used to assess stroke risk in patients with atrial fibrillation [6]. Once the scorecard is completed, it helps to assess the risk factors and help manage and/or treat any controllable risk factors [1].
This study aims to determine the proportion of male patients attending the outpatient department (OPD). This specific group is often overlooked in stroke risk assessment compared to hospitalized patients. By focusing on this specific population, the research seeks to understand the prevalence of stroke risk factors among men seeking outpatient care in this region. Focusing on outpatients allows the study to identify potential stroke risks earlier, enabling preventive interventions. This information can be crucial for developing targeted preventive strategies and raising awareness about stroke risk factors in male patients.
Objectives
1. To assess the proportion of stroke risk among male patients attending the outpatient departments.
2. To determine the association of stroke risk level with socio-personal variables.
Hypothesis
The hypothesis was tested at a 0.05 level of significance.
- HA1: There is a significant association of stroke risk level with socio-personal variables.
- H01: There is no significant association of stroke risk level with socio-personal variables.
- Setting of the study: General Medicine Outpatient Department of MOSC Medical Mission Hospital, Kolenchery, Ernakulam district, Kerala.
- Research approach: Quantitative approach
- Research design: The design used in this study was descriptive-analytical design.
- Sample size: Based on the results of a pilot study the sample size was calculated using my sample size calculation software developed by the Department of Biostatistics. The sampling technique used was the convenience sampling technique. The following formula was used to calculate the sample size.
σ = Anticipated standard deviation (7.02)
Z1-α/2 = 1.96 (at 5% α)
µ = Anticipated mean (87.9)
d = Precision (2%)
The required sample size at a precision of 2% was 280 subjects. 288 subjects were selected for the study.
Sample: The sample size was 288 male patients attending outpatient departments of a tertiary care hospital.
These patients attending the outpatient department (OPD) typically do not have confirmed pathological diagnoses related to the reason for their visit. The OPD serves as a first point of contact for patients seeking medical evaluation and treatment for a variety of concerns such as initial consultation, and chronic disease management such as diabetes mellitus and hypertension.
Sampling technique: Non-probability Convenient sampling technique
Inclusion criteria: The samples were selected based on the following inclusion criteria:
Male patients without any previous history of stroke.
Patients who are able to comprehend Malayalam or English.
Exclusion criteria: The following patients were excluded from the study:
Patients with a previous history of stroke and neurological deficits.
Data collection instruments
Tool 1: Socio-Personal Performa.
It consists of 7 questions for collecting demographic data such as age, education, employment status, family type, financial status, BMI, and place of residence.
Tool 2: Stroke risk scorecard stroke risk scorecard developed by the National Stroke Association was used to assess the proportion of the risk of stroke among male patients. The stroke risk scorecard contains 8 risk factors and is divided into 3 categories, high risk, caution, and low risk, each category is represented with a different colour that is high risk denoted with red colour, caution with yellow and low risk with green colour.
Scoring: The scoring is based on how many factors are identified by the patient in each category. If 3 or more factors are identified in the high-risk category, the patient is at high risk for stroke.
Content validity
To ensure content validity, the tool was submitted to 4 experts in the fields of neuro-medicine, general medicine, and medical-surgical nursing. They were requested to judge the items for their relevance, appropriateness, and degree of agreement for the study. The content validity index was calculated. Items with a content validity index of more than 90% were included in the tool.
Ethical clearance
Initially, the researcher obtained ethical clearance from the Institutional Ethics Committee and permission from administrative authorities of MOSC Medical College Hospital, Kolenchery, and the Head of the Department of General Medicine.
Data collection procedure
After getting permission from the concerned authority, data was collected during the month of March. Investigators identified male patients based on inclusion criteria. After a brief self-introduction, details of the study were explained and consent was taken. Investigators collected data by using socio-personal proforma and stroke risk scorecards to assess the stroke risk, which was read out to them and made provisions to clarify their doubts. Investigators marked the score based on the information provided by the participants. The researcher thanked each subject for their cooperation in the study.
Data were analyzed by descriptive and inferential statistics using Microsoft Excel and R software.
Section A: Frequency and percentage distribution of demographic variables.
The frequency and percentage distribution of demographic variables are shown in Table 1.
| Table 1: Description of demographic variables (n = 288). | |||
| Sl.no | Demographic variables | Frequency (f) | Percentage (%) |
| 1. | Age A) 35-44 |
40 | 13.9% |
| B) 45-54 | 93 | 32.3% | |
| C) 55-64 | 95 | 32.9% | |
| D) 65-74 | 60 | 20.9% | |
| 2. | Education A) Primary |
37 | 12.8% |
| B) Secondary | 89 | 30.9% | |
| C) Higher Secondary | 77 | 26.7% | |
| D) Degree | 85 | 29.6% | |
| 3. | Occupation A) Employed |
106 | 36.9% |
| B) Not employed | 65 | 22.5% | |
| C) Self-employed | 117 | 40.6% | |
| 4. | Religion A) Christian |
158 | 54.8% |
| B) Hindu | 91 | 31.6% | |
| C) Muslim | 39 | 13.6% | |
| 5. | Family A) Nuclear family |
187 | 64.8% |
| B) Joint family | 101 | 35.2% | |
| 6. | Financial status A) Above poverty line |
215 | 74.6% |
| B) Below poverty line | 73 | 25.4% | |
| 7. | BMI A) < 18 |
30 | 10.5% |
| B) 18-23 | 134 | 46.5% | |
| C) > 23 | 124 | 43.0% | |
| 8. | Place of residence A) Rural area |
183 | 63.5% |
| B) Urban area | 105 | 36.5 % | |
Section B: Analysis and interpretation of risk of stroke among male patients
Table 2 shows the frequency and percentage of stroke risk among male patients.
| Table 2: Frequency and percentage of stroke risk among male patients (n = 288). | ||
| Stroke Risk | Frequency | Percentage |
| Low | 125 | 43.4% |
| Caution | 40 | 13.9% |
| High | 123 | 42.7% |
| Total | 288 | 100% |
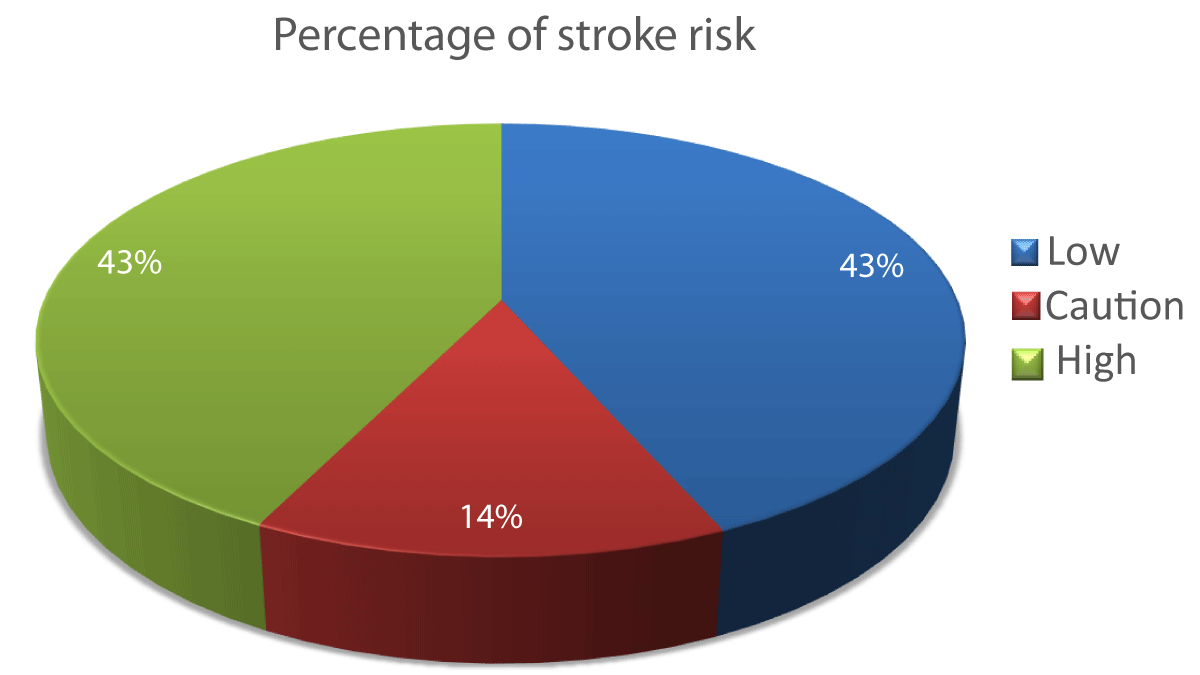
The pie diagram (Figure 1) shows that 43.4% have low stroke risk and 42.7% have high risk.
Figure 1: Pie diagram showing the percentage of stroke risk among male patients.
Section C: Association of stroke risk level with demographic variables
A chi-square test was done to find the association between stroke risk level with socio-personal variables. There is a significant association of stroke risk level with age, education, occupation, BMI, and place of residence. (Table 3).
| Table 3: Association of stroke risk level with demographic variables (n = 288). | ||||||
| Sl.no | Demographic variables | Risk of stroke | Chi-square | p - value | ||
| Low | Caution | High | ||||
| 1. | Age A) 35-44 |
26 | 5 | 9 | 33.03 | 0.00* |
| B) 45-54 | 53 | 11 | 29 | |||
| C) 55-64 | 35 | 14 | 46 | |||
| D) 65-74 | 11 | 10 | 39 | |||
| 2. | Education A) Primary |
11 | 9 | 17 | 14.91 | 0.021* |
| B) Secondary | 30 | 11 | 48 | |||
| C) Higher Secondary | 37 | 10 | 30 | |||
| D) Degree | 47 | 10 | 28 | |||
| 3. | Occupation A) Employed |
52 | 16 | 38 | 15.13 | 0.004* |
| B) Not employed | 16 | 14 | 35 | |||
| C) Self-employed | 57 | 10 | 50 | |||
| 4. | Religion A) Christian |
72 | 16 | 70 | 6.93 | 0.139 |
| B) Hindu | 40 | 14 | 37 | |||
| C) Muslim | 13 | 10 | 16 | |||
| 5. | Family A) Nuclear family |
82 | 20 | 85 | 4.88 | 0.087 |
| B) Joint family | 43 | 20 | 38 | |||
| 6. | Financial status A) Above poverty line |
98 | 29 | 88 | 1.65 | 0.437 |
| B) Below poverty line | 27 | 11 | 35 | |||
| 7. | BMI A) < 18 |
22 | 0 | 8 | 52.27 | 0.00* |
| B) 18-23 | 78 | 17 | 39 | |||
| C) >23 | 25 | 23 | 76 | |||
| 8. | Place of residence A) Rural area |
88 | 27 | 68 | 6.42 | 0.040* |
| B) Urban area | 37 | 13 | 55 | |||
Our study investigated the association between stroke risk and various factors in male outpatients attending a tertiary care hospital in Ernakulam, Kerala. As hypothesized (HA1), the analysis revealed significant associations between stroke risk and age, education, occupation, body mass index (BMI), and place of residence. These findings offer valuable insights into the stroke risk profile of this specific male outpatient population.
Age
The positive association between age and stroke risk aligns with established knowledge [7]. As men age, physiological changes and the accumulation of risk factors like hypertension and atherosclerosis contribute to an increased vulnerability to stroke.
Education
The observed link between lower education and higher stroke risk is consistent with previous research [8]. Lower educational attainment might be associated with limited access to healthcare information, unhealthy lifestyle choices, and socioeconomic disadvantages that increase stroke risk.
Occupation
The association between occupation and stroke risk suggests a potential role of occupational exposures or physical demands in stroke risk. Further investigation into specific occupations with high stroke risk could be beneficial for targeted preventive strategies.
Body Mass Index (BMI)
The positive association between BMI and stroke risk is well-documented [9]. Excess weight contributes to various conditions like hypertension and diabetes, which are major risk factors for stroke.
Place of residence
The observed association between place of residence and stroke risk warrants further exploration. Potential factors like access to healthcare, dietary habits, and environmental exposures in different residential areas could be influencing stroke risk.
Limitations
Our study has some limitations. Data on established risk factors like smoking history, blood pressure, cholesterol levels, and diabetes were not collected, potentially underestimating the true stroke risk burden. Additionally, the study focused on a single hospital in a specific region, limiting the generalizability of the findings.
Future directions
Future research should incorporate a broader range of established stroke risk factors to provide a more comprehensive picture. Studies across diverse geographic locations with larger sample sizes could enhance the generalizability of the results. Investigating the specific mechanisms behind the observed associations between occupation and place of residence could inform targeted preventive interventions.
This study identified significant associations between stroke risk and age, education, occupation, BMI, and place of residence among male outpatients. These findings highlight the importance of considering these factors in stroke risk assessment and prevention strategies for this population subgroup. Further research addressing the limitations can provide more comprehensive insights and guide the development of effective preventive measures to reduce the stroke burden.
Here we extend our sincere thanks to all the study participants who participated in the study.Here we extend our sincere thanks to all the study participants who participated in the study.
- Sacco RL, Kasner SE, Broderick JP, Caplan LR, Connors JJ, Culebras A, Elkind MS, George MG, Hamdan AD, et al. American Heart Association Stroke Council, Council on Cardiovascular Surgery and Anesthesia; Council on Cardiovascular Radiology and Intervention; Council on Cardiovascular and Stroke Nursing; Council on Epidemiology and Prevention; Council on Peripheral Vascular Disease; Council on Nutrition, Physical Activity and Metabolism. An updated definition of stroke for the 21st century: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013 Jul;44(7):2064-89. doi: 10.1161/STR.0b013e318296aeca. Epub 2013 May 7. Erratum in: Stroke. 2019 Aug;50(8):e239. PMID: 23652265.
- Stroke Networks. Home - Stroke Networks. Stroke Networks. https://strokenetwork.org/
- Diwakar AM. A study to assesss the awareness of risk factors and warning signs of stroke among patients in selected hospital, Ludhiana, and Punjab. International journal of nursing care. 2014; 2(1): 1-5.
- Strong K, Mathers C, Bonita R. Preventing stroke: saving lives around the world. Lancet Neurol. 2007 Feb;6(2):182-7. doi: 10.1016/S1474-4422(07)70031-5. PMID: 17239805.
- Shah RS, Cole JW. Smoking and stroke: the more you smoke the more you stroke. Expert Rev Cardiovasc Ther. 2010 Jul;8(7):917-32. doi: 10.1586/erc.10.56. PMID: 20602553; PMCID: PMC2928253.
- Fuster V, Rydén LE, Cannom DS, Crijns HJ, Curtis AB, Ellenbogen KA, Halperin JL, Kay GN, Le Huezey JY, Lowe JE, Olsson SB, Prystowsky EN, Tamargo JL, Wann LS, Smith SC Jr, Priori SG, Estes NA 3rd, Ezekowitz MD, Jackman WM, January CT, Lowe JE, Page RL, Slotwiner DJ, Stevenson WG, Tracy CM, Jacobs AK, Anderson JL, Albert N, et al. American College of Cardiology Foundation/American Heart Association Task Force. 2011 ACCF/AHA/HRS focused updates incorporated into the ACC/AHA/ESC 2006 guidelines for the management of patients with atrial fibrillation: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2011 Mar 15;123(10):e269-367. doi: 10.1161/CIR.0b013e318214876d. Epub 2011 Mar 7. PMID: 21382897.
- GBD 2016 Lifetime Risk of Stroke Collaborators; Feigin VL, Nguyen G, Cercy K, Johnson CO, Alam T, Parmar PG, Abajobir AA, Abate KH, Abd-Allah F, Abejie AN, Abyu GY, Ademi Z, Agarwal G, Ahmed MB, Akinyemi RO, Al-Raddadi R, Aminde LN, Amlie-Lefond C, Ansari H, Asayesh H, Asgedom SW, Atey TM, Ayele HT, Banach M, Banerjee A, Barac A, Barker-Collo SL, Bärnighausen T, Barregard L, Basu S, Bedi N, Behzadifar M, Béjot Y, Bennett DA, et al. Global, Regional, and Country-Specific Lifetime Risks of Stroke, 1990 and 2016. N Engl J Med. 2018 Dec 20;379(25):2429-2437. doi: 10.1056/NEJMoa1804492. PMID: 30575491; PMCID: PMC6247346.
- Otite FO, Liaw N, Khandelwal P, Malik AM, Romano JG, Rundek T, Sacco RL, Chaturvedi S. Increasing prevalence of vascular risk factors in patients with stroke: A call to action. Neurology. 2017 Nov 7;89(19):1985-1994. doi: 10.1212/WNL.0000000000004617. Epub 2017 Oct 11. PMID: 29021359; PMCID: PMC5679417.
- Yusuf S, Hawken S, Ounpuu S, Bautista L, Franzosi MG, Commerford P, Lang CC, Rumboldt Z, Onen CL, Lisheng L, Tanomsup S, Wangai P Jr, Razak F, Sharma AM, Anand SS; INTERHEART Study Investigators. Obesity and the risk of myocardial infarction in 27,000 participants from 52 countries: a case-control study. Lancet. 2005 Nov 5;366(9497):1640-9. doi: 10.1016/S0140-6736(05)67663-5. PMID: 16271645.