More Information
Submitted: February 08, 2024 | Approved: March 21, 2024 | Published: March 25, 2024
How to cite this article: Daniel ES, Collie L, Neymour A, Martin-Chen NKA, Moss K, et al. Factors Influencing Knowledge on the Completion of Treatment among Tuberculosis Patients under Directly Observed Treatment Strategy (DOTS) in a Selected Health Facility, the Bahamas. Clin J Nurs Care Pract. 2024; 8: 022-030.
DOI: 10.29328/journal.cjncp.1001053
Copyright License: © 2024 Daniel ES, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Tuberculosis; DOTS; Adherence; Knowledge; Influencing factors
Factors Influencing Knowledge on the Completion of Treatment among Tuberculosis Patients under Directly Observed Treatment Strategy (DOTS) in a Selected Health Facility, the Bahamas
Esther S Daniel1*, Latasha Collie2, Alice Neymour2, Nicole KA Martin-Chen3, Kevin Moss4, Kathy-Ann Lootawan1 and Virginia M Victor1
1KThe UWI School of Nursing, Faculty of Medical Sciences, The University of the West Indies, Trinidad and Tobago
2Department of Public Health, Ministry of Health, Nassau, Bahamas New Providence
3Ministry of Health and Wellness Technical Services, National Epidemiology Branch, Jamaica
4Department of Medicine, Public Hospital Authority, Ministry of Health, Nassau, Bahamas New Providence
*Address for Correspondence: Esther S Daniel, The UWI School of Nursing, Faculty of Medical Sciences, The University of the West Indies, Trinidad and Tobago, Email: [email protected]
Objective: To determine the factors influencing completion of DOTS in Tuberculosis treatment in the Bahamas.
Methods: A quantitative, descriptive cross-sectional survey. Tuberculosis patients aged 18 years and above were considered regardless of the site or the smear status of their TB. The sample size was 40. Data analysis and interpretation were done using the statistical package for the social sciences software (SPSS version 24), through the exploration and calculation of descriptive (frequencies, percentages, means, standard deviations, and inferential (Anova) statistical methods. Statistical significance was determined to be a p < 0.05.
Results: The mean age of the respondents, was 39.9 years, SD 11.65, and 73% of them were men. 63% of participants, 78% of whom were citizens of the Bahamas, reported having no annual income. Seventy-eight percent (31) of the participants said they had insufficient food and drink while they were unwell. More than half of the participants in the survey reported being on at least one pharmaceutical regimen, although 36% said they were not actively taking any of the prescription medications.
Conclusion: Less than a third were noncompliant with DOTS, this was influenced by factors such as annual income, no family support, marital status, employment status, and educational level.
1.6 million persons worldwide passed away from TB in 2021. (including 187,000 people with HIV). Following COVID-19 (behind HIV/AIDS), TB is the second infectious killer in the world and the 13th largest cause of death overall. Many people today assume that Tuberculosis (TB) is a disease of the past, but it is not. It continues to be a significant global health problem [1].
Eighty-seven percent of new TB cases in 2021 were found in the 30 countries with the highest TB burden. Multidrug-resistant tuberculosis (MDR-TB) continues to be a public health emergency and a security risk to health. In 2020, just around one in three individuals with drug-resistant TB received therapy [1].
The Commonwealth of the Bahamas is an archipelagic nation of approximately 700 islands and 2,400 cays and rocks, with a landmass of 13,878 km2 spread across 259,000 km2 of the ocean. The main islands are Grand Bahamas and New Providence, where the capital, Nassau, is located [Appendix E]. However, the mid-2019 census states that the population in The Bahamas is projected to be approximately 390,000 people [2].
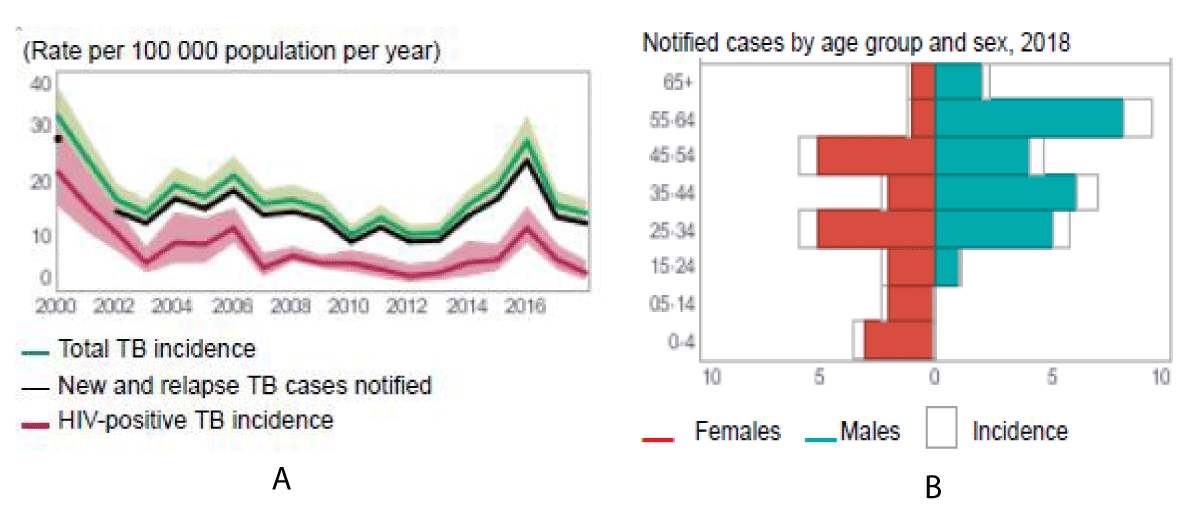
The Bahamas is no different from any other Caribbean Island (Graph A&B) that has this disease, which is a potentially life-threatening infection, especially for persons whose immune system has been compromised.
Graph A & B: The Graphs illustrate the TB incidence rates per 100,000 population per year and notified cases by age group within the Bahamas (Appendices).
Because TB is a health problem classified as a communicable disease, the health system is responsible for controlling and preventing its introduction and spread. In this study, the researchers evaluated factors such as ignorance (poor health literacy), transportation barriers, alcohol, and substance abuse, as well as stigma among others that are possibly the principal influence of compliance with the Direct Observation Treatment Short Course (DOTS) in such respondents.
The Government of the Bahamas has since embarked on thorough screening of patients, effective measures have been put in place for treatment upon screening and diagnosis. However, like so many other countries in the world, The Bahamas still must deal with cases of non-compliance with the DOTS Program.
Tuberculosis remains the world’s leading cause of death from an infectious agent, exceeding human immunodeficiency virus/acquired immune deficiency syndrome (HIV/AIDS) for the first time [3]. TB is an Opportunistic Infection (OI) that occurs more often or is more severe in people with weakened immune systems than in people with healthy immune systems. Therefore, people who have contracted the Human Immuno-Deficiency Virus (HIV) have proven to have a higher percentage of patients contracting the TB bacteria. This is only because HIV weakens the immune system thus increasing the risk of TB in people with HIV [4].
Although the disease is curable, infected persons must consistently take the antibiotics daily for the prescribed period. Fundamentally, these respondents must strictly adhere to the treatment of TB to get effective outcomes [4]. Infected patients must incur costs of treatment, diagnosis, transportation back and forth to the medical facilities as well as the opportunity costs of the time used for treatment. When adequately treated, the initially infected person heals from the disease.
On the other hand, some respondents do not maintain consistency with the treatment, thus leading to the development of drug-resistant TB [5]. While some respondents relapse, a significant number of them develop resistance to treatment. According to medical scholars, Multi-Drug Resistant and Extensive Drug Resistant Tuberculosis (MDR-TB and XDR-TB), coupled with HIV and weak immune systems are the principal hindrances to the effective treatment of tuberculosis [5].
The researchers argue in this paper that respondents’ literacy level, drug, and substance abuse, extent of feeling better, and transportation costs, amongst other factors, play a critical role in the completion of medical treatment for tuberculosis among respondents. Therefore, the Failure of respondents to complete their treatment has been a huge problem in the medical facilities [6].
In 1492, Christopher Columbus landed in The Bahamas, initiating his discovery of the New World and bringing with him a dreaded new disease-Tuberculosis (TB). In 1949, the Chest Clinic (outpatient follow-up care) was established; and in 1959, contact-tracing along with a register, was implemented [2]. In 1955, thereafter, The Bahamas General Hospital was renamed Princess Margaret Hospital. These developments led to a Chest Wing (1962) which included, a wing for private TB patients, a floor with 3 wings for female respondents, and a floor with 3 wings for male respondents and a wing for children, on the ground floor [2]. The Chest Clinic is in the Paediatrics Corridor, upstairs at the Out-Patient Department, Princess Margaret Hospital. Once they are diagnosed with positive cases of TB in the hospital and discharged, they are followed up in their communities [2].
Despite this extensive service coverage, however, the program performance indicators remain unsatisfactory to declare The Bahamas Tuberculosis Free thus the TB control program cannot be successful with extensive service availability alone.
Pulmonary Tuberculosis is curable under the principle of early, combined, regular, and completion of treatment. Subsequently, when treatment compliance directly affects the treatment effect, as well as treatment interruption it can lead to increased risk of drug resistance in these patients. According to the World Health Organization, Tuberculosis is one of the top 10 causes of death worldwide, therefore, it is reflected as the leading cause of death from a single infectious agent. In 2020, there were an estimated 10 million new cases of Tuberculosis, whereas 1.5 million people died from this disease [3].
On a global level, there are many factors that influence Tuberculosis treatment completion such as access to quality drugs. In many countries, the quality of tuberculosis medication is poor, because of this it can lead to treatment failure and non-completion of treatment. Tuberculosis is often misdiagnosed or not diagnosed at all and this happens when there is no availability of diagnostic testing which can cause treatment to be delayed or not started at all. Finally, there is adherence to treatment, the success of tuberculosis treatment depends on the patient taking their medication correctly and consistently by not carrying out this task they will encounter challenges in some parts of the world [3].
Across the globe and in the Bahamas, the administration of the Direct Observation Therapy Short course for TB has reduced the prevalence of the disease on a significant scale. However, its impact in reducing TB incidence has been limited by non-compliance to DOTS which occurs when patients do not turn up for treatment either at the health facility or community DOT point [7]. Subsequently, in some countries where DOTS have had little impact on TB control, poor or non-compliance to self-administered TB treatment is common and has been identified as an important cause of failure of initial treatment, leading to relapse. Notwithstanding, some respondents have been failing to adhere to the treatment, causing relapse, resistance to TB therapy, and in the worst-case scenario, death of the infected persons. Despite the studies on factors influencing non-adherence to TB therapy being conducted and published across the globe, little has been done in the West Indies and the Bahamas [8]. The research thus delves into studying and analyzing the factors behind non-compliance with TB treatment in the Bahamas.
A study from Nigeria found that distance from a DOTS center, insufficient knowledge of TB, and multiple care-seeking contributed to the delay. Multiple care-seeking was defined as visiting one or more non-DOTS centers for treatment before going to a DOTS facility. The delay was conceptualized as taking more than 28 days from the first onset of symptoms to visit a DOTS center [9].
A similar study was carried out in Zambia by Kaona, et al. The study sought to understand the factors that significantly impacted adherence to treatment as well as knowledge of the transmission routes of TB among patients [10]. Interestingly, the researchers found that age, marital status, and level of education were not significant factors in determining whether a patient was likely to adhere to the entire DOTS regimen of medication. Rather, the study determined that four factors caused non-compliance with the entire medication course, including the strength of the drugs, lack of medication at home, insufficient knowledge of the benefits of completing the full DOTS medication regimen, and patients beginning to feel better before they have taken all their medication [10].
In a study by Sanneh and Pollock carried out in Gambia, the researchers sought to compare outcomes before and after DOTS treatment [11]. A second arm of the study sought to qualitatively measure the knowledge and attitudes of those who defaulted on treatment. The quantitative arm of the research did not find any significant difference in the outcomes of patients when comparing pre-DOTS and post-DOTS outcomes. The outcomes were measured using cured, out of control, complete treatment, treatment failure, and death as the primary outcome variables. The qualitative arm of the study interviewed the people who prematurely terminated treatment. The study found that among this group, the vast majority had insufficient knowledge about TB, its causes, symptoms, transmission, and treatment. As a result, the patients did not immediately seek treatment at a DOTS facility for an average of three weeks (which is how long it took for them to get a definitive diagnosis of TB), and this period could extend up to years [11]. Therefore, knowledge of TB and its treatment is a significant factor affecting compliance and full treatment.
A study carried out by Bam, et al. in urban Kathmandu found that older people (those above 54 years) were twice as likely to prematurely stop treatment as their younger counterparts. Moreover, widowed or divorced participants were more likely to prematurely stop treatment than either their single or married counterparts regardless of age (50% compared to 17.5% and 27.8% of respondents respectively) [12]. Regarding adherence, the researchers found that the most common reasons were that the patients had not been told to take the medication regularly and that they thought that they had been cured when they began to feel better.
Mushtaq et al conducted a study in the Punjab province of Pakistan that yielded interesting results regarding knowledge of TB. However, Mushtaq, et al. noted that it is important for the general population to be educated about TB before contracting it to reduce delays and increase the participation of patients in the DOTS treatment until completion. After all, it is evident from observation that individuals who have contracted and have been diagnosed with a disease are more likely to know detailed information about it than people who have not. Thus, assessing the levels of knowledge – and the factors affecting the acquisition of this knowledge – in the general population is important as well. Eighty-one percent (81%) of urban dwellers knew that TB was transmitted through the air when a patient sneezes or coughs. In contrast, only 68.5% of people in the rural district knew this. Considering that a chronic cough is the most common symptom (and, thus, the most well-known), the differences increased when it came to knowledge about lesser-known symptoms. Regarding treatment, the vast majority of both urban and rural dwellers knew that treatment was by medication and it could be sought at government or private medical facilities. However, fewer people in both groups knew that the duration of treatment was 6 to 9 months (69.2% of urban sample versus 54.9% of rural dwellers) [13].
An other aspect that may affect knowledge of the treatment, symptoms, transmission, and DOTS of tuberculosis is gender. One study carried out in rural China showed by Wang, et al. sought to determine whether there were any gender differences in the knowledge of TB and health-seeking behaviors. The study notes that gender disparities are cross-sectional when they occur, meaning that they have impacts that cut across socio-economic indicators, including income, employment, literacy, and health care [14].
There are numerous factors that can affect the knowledge that people have regarding DOTS, the preferred treatment regimen for TB. Such factors include age, gender, marital status, family type, income, occupation, and residence among others. One major discovery is the dearth of literature that examines the impact of socio-demographic factors on knowledge of TB and its treatment from a Bahamian perspective. It is vital to the health care of the nation that a body of work is built to examine this particular aspect of the issue. The current research seeks to contribute to this body of work. The socio-demographic factors identified above in other regions and locations indicate that knowledge of TB treatment and DOTS can be impacted by various factors. As such, it is worth investigating these factors in a local setting to determine how best to approach the education of the public regarding TB and its treatment through DOTS.
Study site
The present study was the first to be conducted in Bahamas New Providence, in the community covered by the Public Hospital Authority (PHA), Bahamas. PHA is a quasi-government-owned premier, acute tertiary care facility. TB patients aged 18 years and above were considered regardless of the site or the smear status of their TB. To be eligible for this study, patients needed to have taken anti-TB treatment at least for a month. The hospital, including the TB clinic, was established in the year 1999 by an act of The Bahamas parliament [15]. The TB clinic offers services in the screening of TB, administration of DOTS, and other treatment services to respondents suffering from TB.
Study design
A descriptive, quantitative, and cross-sectional study.
Study population
TB patients aged 18 years and above were considered regardless of the site or the smear status of their TB. To be eligible for this study, patients needed to have taken anti-TB treatment at least for a month.
Variables
Variables of the study included Dependent Variable (DV): Knowledge on completion of treatment for Tuberculosis. This refers to whether or not participants had significant knowledge of the importance and benefits of completing the DOTS regimen. Attributed Variable (AV): Age, gender, level of education, number of dependents, marital status, nationality, annual income, and employment status.
Sample size estimation
The study utilized the TB patients whose names had been entered in the TB registry (2019) at the Chest Clinic in the Bahamas and have been confirmed from aliments through scientific clinical tests in the laboratory. The total population of Nassau – 390,000. The total number of patients diagnosed and confirmed (sputum positive) patients was 43. The number of patients who were defaulters was 19, a total of 62. As per exclusion criteria defaulters (19), hospitalized patients (2), and the dead (1) were excluded from the study. The sample size included confirmed patients on DOTS treatment was 40.
Ethics approvals
Ethical approval was obtained from the UWI Campus Ethics Committee and the college Ethics Board to conduct the study. Subjects of this research study had the right to consent freely without coercion. Furthermore, they were offered the right to refuse to participate or withdraw at any time without explanation, consequences, or coercion.
Instrument
A self-administered questionnaire was used to collect data– socio-demographic data (12 items), Clinical characteristics - 12 items, Health care systems -- 8 items, Knowledge -- 7 items, during the months of July and August. Data was verified and coded by the researcher. SPSS statistical software was used for data entry, management, and analysis. To minimize data entry errors, check codes were incorporated into the database and the data was cleaned to ensure consistency of responses.
The TB patients' right to anonymity, privacy, and confidentiality was respected by obtaining consent from all and respecting any additional requests for privacy and confidentiality identified by each of them. Storing all information securely and de-identifying the source of specific information in the final project. In order to minimize risk to subjects, data sets were coded. A wide variety of methods were used to code data. The numbers were sequential, they were hashed from a sequential number, and they were randomly assigned. Even though the Code number was unique, and the subject was not readily identifiable, the dataset cannot be claimed to be de-identified, and protections were applied when sharing the data. An investigator obtained individually identifiable information on the treatment outcomes of patients treated for Tuberculosis with either Drug A or Drug B by viewing patients’ existing individually identifiable medical records at the clinics where the patients were being treated. The investigator recorded only the patient's age, gender, diagnosis, treatment, and health status at the end of 6 months of treatment so that the investigator could not link the recorded information back to the patients. In this study, the investigator conducted human subjects research because the investigator obtained identifiable private information from patients since the investigator records the information in such a manner that subjects cannot be identified either directly or indirectly through identifiers linked to the subjects.
The theoretical framework
The theoretical framework used in the study was built on the concept of Social Determinants of Health (SDH) framework. The concept of social determinants has been extensively examined in many literatures. At its core, the concept asserts that economic and social conditions are the primary reason behind differences between individuals and among groups [16]. According to data, socioeconomic determinants of health are to blame for at least 50% of a population's health losses. Non-medical factors that influence health outcomes are known as social determinants of health [16].
At Tehran University of Medical Sciences, a prospective cohort study on the social determinants of health was carried out. At various socioeconomic levels, the relationship between the Social Determinants of Health (SDH) and other health risk factors and outcomes was assessed. Multiple models and confounding effect control were used to explore the relationship between independent factors and health (either objective or subjective) [17].
The study’s theoretical framework hypothesizes how socio-demographic factors affect a person’s level of knowledge regarding TB treatment (that is, DOTS). Studies have shown that level of knowledge is a significant factor in predicting adherence, and that people with insufficient information about the disease are more likely to prematurely stop taking medication just because they feel better after some time. The effectiveness of DOTS is predicated on the completion of the 6-to-9-month medication regimen, and the completion of the regimen is predicated on patients being aware of the disease and the benefits of a full course of treatment. In view of this, it is important to understand how socio-demographic factors can impact one’s knowledge of TB.
Data analysis
Data were verified and coded by the researcher. SPSS statistical software Version 24 was used for data entry, management, and analysis. To minimize data entry errors, check codes were incorporated into the database and the data were cleaned to ensure consistency of responses. After data, entry each form was checked on the database twice by two different members of the research team to verify that the information was accurate. These checks include checks for misspellings, entries missing numbers, etc., and inaccuracies corrected, additionally, frequency tables were run in SPSS to also verify the information entered and this was done by two separate members of the team.
Data were analyzed using frequencies, means, proportions, standard deviations, and percentages. Factors associated with the completion of treatment of TB under the DOTS strategy were analyzed. Interpretation of the data was visualized through the exploration and calculation of descriptive (frequencies, percentages, means, standard deviations, and inferential (Anova) statistical methods. Statistical significance was determined to be a p - value of ≤ 0.05. Data was presented in the form of tables and graphs.
Ethical considerations
Ethical approval was obtained from the UWI Campus Ethics Committee, St Augustine, and UWI Ethics Committee located in Nassau, The Bahamas to conduct the research. Once approval was received from the ethics committee, the researcher wrote to the Permanent Secretary and Director of Nursing at the Ministry of Public Health to seek permission to collect data from the patients at the Chest Clinic located in Nassau, the Bahamas. Upon grant of approval, the researcher met with the respondents and invited them to participate in the study. Informed consent was obtained from each respondent who agreed to be in the study.
Subjects of this research study had the right to consent freely in the absence of coercion. They were offered the right to refuse to participate, or to withdraw at any time with no explanation, and without consequences or coercion of any kind.
The analysis of the results showed that (Table 1). Tuberculosis patients who reported being on the directly observed therapy for the treatment and receiving follow-up care by health care staff in the Bahamas, indicated that most participants on DOTS were over forty years old (58%), male (73%), single (73%), Bahamian (78%), obtained a secondary education (63%), and unemployed (55%). Similarly, those who reported receiving regular follow-ups by health care facility staff were over forty years old, male, single, having obtained a secondary education, and were unemployed. Amongst participants seventy-eight percent, (31) reported having insufficient food and water supplies during the duration of illness. Seventy-three percent, (29) had experienced stigma because of their Tuberculosis diagnosis, whilst sixty-three percent, (25) had received family support and fifty-eight percent, (23) had discussed their illness with family members (Table 2).
| Table 1:Demographic Characteristics of TB patients on DOTS, at a Health Facility in the BahamasN = 40. | ||||
| Direct Observed Therapy for the Treatment of Tuberculosis (DOTS) | ||||
| Characteristic | Frequency | Percentage | ||
| Yes | No | Yes | No | |
| Age Group | ||||
| Under 40 years | 17 | 0 | 42.5% | 0% |
| Over 40 years | 23 | 0 | 57.5% | 0% |
| Total | 40 | 0 | 100% | 0% |
| Gender | ||||
| Male | 29 | 0 | 72.5% | 0% |
| Female | 11 | 0 | 27.5% | 0% |
| Total | 40 | 0 | 100% | 0% |
| Marital Status | ||||
| Married | 11 | 0 | 27.5% | 0% |
| Single | 29 | 0 | 72.5% | 0% |
| Total | 40 | 0 | 100% | 0% |
| Direct Observed Therapy for the Treatment of Tuberculosis (DOTS) | ||||
| Characteristic | Frequency | Percentage | ||
| Yes | No | Yes | No | |
| Nationality | ||||
| Bahamian | 31 | 0 | 77.5% | 0% |
| Haitian | 9 | 0 | 22.5% | 0% |
| Total | 40 | 0 | 100% | 0% |
| Highest Educational Level Obtained | ||||
| Secondary | 25 | 0 | 62.5% | 0% |
| Vocational School | 9 | 0 | 22.5% | 0% |
| College | 6 | 0 | 15.0% | 0% |
| Total | 40 | 0 | 100% | 0% |
| Employment Status | ||||
| Employed | 3 | 0 | 7.5% | 0% |
| Unemployed | 22 | 0 | 55.0% | 0% |
| Self-employed | 15 | 0 | 37.5% | 0% |
| Total | 40 | 0 | 100% | 0% |
| *N = Frequency, % = Percentage. | ||||
| Table 2: Specific Socioeconomic Demographic Characteristics, of TB respondents at a health facility in the Bahamas N = 40. | ||||||||
| Yes | Sometimes | No | Total | |||||
| N | % | N | % | N | % | N | % | |
| Insufficient nutrition | 31 | 77.5 | 4 | 10 | 5 | 12.5 | 40 | 100 |
| Experienced Stigma | 29 | 72.5 | 0 | 0.0 | 10 | 25.0 | 39 | 100 |
| Family support | 25 | 62.5 | 12 | 30.0 | 3 | 7.5 | 40 | 100 |
| Discussed sickness with family | 23 | 57.5 | 0 | 0.0 | 17 | 42.5 | 40 | 100 |
| Total | 108 | 67.9 | 16 | 10.0 | 35 | 22.1 | 159 | 100 |
| *N = Frequency, % = Percentage. | ||||||||
Analyses of clinical characteristics of study respondents clinical characteristics
DOTS and follow up health care facility: Tuberculosis patients mostly reported receiving regular follow-ups (35,88%) by health care facility staff and being on the DOTS (40, 100%) treatment program for the duration of their illness. Tuberculosis patients who participated in the study predominantly (28,70%) reported being on a six-month treatment for their illness.
The members of the study population were mostly unable to recall (8, 20%) their actual date of tuberculosis diagnosis. More than half of the study population reported being on at least one of the prescribed medication regimens, however, thirty-six percent reported not being prescribed currently any of the indicated medications.
The participating cohort reported a cough for more than two weeks as their most common symptom preceding their tuberculosis diagnosis. Hypertension was the most commonly diagnosed other condition amongst the study population (11, 57.9%) and with (12,63.2%) of participants reportedly being prescribed antihypertensive medication, all participants reported not being currently pregnant (40,100%), equal portions reported a history of smoking and (24, 60%) alcohol consumption. Most participants reported weekly (24,60%) consumption of alcohol, with daily (3, 12.5%) consumption being the least reported frequency.
Analyses of perceptions of health care systems: The study population's perceptions of the health system, in the Bahamas upon examination revealed no significant variance in positive or negative responses within or between nationalities. However, having to travel back and forth for clinical appointments (F (1,35) = 3.305, p = 0.078), and always keeping scheduled appointments (F (1,35) = 3.104, p = 0.087), demonstrates a possibility of variance in responses among nationality. The study population demonstrated a statistically significant effect between gender responses to the statements “I run short of medication” (F (1,35) = 4.053, p = 0.052), and “Health care received from Health care providers on Tuberculosis”, (F (1,35) =4.950, p = 0.033)
There was no statistically significant effect of Tuberculosis patients’ marital status on their responses regarding the healthcare system in the Bahamas. There was no significant effect of a TB patient’s educational status on their response regarding the health care system in the Bahamas. The employment status of study participants demonstrated variable effects in positive and negative responses regarding the health care system, with their being significant effect applied regarding the statement “health care providers articulate the need for treatment and importance of compliance”, (F (2,34) = 5.682, p = 0.007).
There was a significant effect reported between the income brackets of TB Patients in comparison to their responses to the statements “I travel back and forth for clinic appointments [F (3,33) = 3.495, p = 0.026)” and “HCP are positive in their attitude towards me. [F (3.33) = 2.081, p = 0.030)”.
Analyses of knowledge of completion of treatment among Tuberculosis study populations beliefs and knowledge regarding Tuberculosis: The study population believed that germs (33,83%) were the predominant source of tuberculosis infection, with all agreeing that heredity (40,100%) and smoking (40,100%) were not sources of Tuberculosis infection. Ninety-eight percent (39) of participants reported that tuberculosis infections' primary mode of spread was airborne. Eighty-eight percent (35) of the TB patient cohort reported that covering one’s mouth and nose when sneezing and coughing was an effective way to stop the spread of Tuberculosis. The lung (29, 73%) was the organ reportedly most affected by Tuberculosis according to the TB patient cohort. A cough for two weeks or more with a fever (35,88%) was the most common symptom reported among the patient cohort. More than half of the participating cohort reported a treatment length (duration) of six (6) months. Vomiting (29,73%) was the most commonly reported Tuberculosis drug side effect amongst the cohort.
The findings from this study conducted at a health facility in the Bahamas, are similar to the literary work existing on the subject matter [2,3,18-21].
Discussions related to demographic, and socio-economic characteristics
As indicated the results identified despite the population size, are similar to those found in other studies. These studies argued that Tuberculosis patients were found typically mostly to be male, country nationals, over forty years old, unmarried (single), unemployed with no income, and having obtained the minimum educational level [2,3,18-21].
Additionally, access to sufficient food supplies, family support, and experiencing stigma and discrimination, offers further insight into how these participants cope through therapy and effectual adherence or non-adherence. As the literature suggests once clients experience low levels of stigma, have adequate family support and food, and are managed effectively with medication; adherence will be greatly improved. This is confirmed by these presented findings as all of the study population reported being on DOTS therapy, with more than half confirming receiving regular follow-up by health facility staff [2,3,18-21]. This further adds to the importance of the role of healthcare providers in influencing and impacting compliance and intended health outcomes.
Alcohol consumption and history of smoking are significant influences as well, and programs to address the presence or potential for abuse in these instances are important. In fact, the literature states that clients who smoke and consume high quantities of alcohol are at a greater risk not just of developing other conditions, but report lower adherence rates to DOTS [2,3,18-21]. Hence the reoccurrence of similar findings suggests that family support and addressing drug abuse is critical in improving a client’s compliance.
Discussions related to clinical characteristics of study respondents
It is common to find that patients receiving treatment for Tuberculosis had preceding symptoms that trigger initiation of care, and also report the presence of other chronic health conditions such as diabetes, HIV, and hypertension. Therefore, these factors influence the delay or early access to healthcare services and the potential for compliance [22]. These findings are intuitive and provide much-needed further insights into the linkages existing between delayed access and early initiation of care and afford possible trigger points for action.
Discussion related to knowledge of completion of treatment among tuberculosis patients on DOTS treatment strategy
Some pundits argue that compliance levels amongst Tuberculosis patients are linked to poor knowledge and belief systems and form the core of the continual spread currently experienced [20].
However, this study proposes an alternate influencing factor tied more to that of a socioeconomic nature, which determines a client’s ability to keep scheduled appointments and internalize the health information provided. In fact, as more than half the cohort were unemployed, with no income and males, it would follow that missing appointments and travel to and from home would be crucial points of variance among participants.
Implications
Nursing education: This study has provided a wealth of insight from the perspective of TB patients' experiences with the completion of DOTS, which has implications for nursing education, practice administration, and research going forward, which is crucial in achieving and maintaining 100% compliance.
Nurses play a crucial and integral role as educators, motivators, and supporters of patients and their families, which is indelibly linked to ensuring their overall health and well-being. In fulfilling this vital role nurses will be required to continue to strengthen their competence in patient TB education and be able to individually motivate patients irrespective of their socioeconomic situation or educational level. They need to be also sensitive to the barrier that a patient’s economic circumstances have on their compliance with treatment.
Nursing practice: As nurses provide care to their patients this heightened sensitivity to the limitations or barriers to care that their patients face, will guide them for more sympathetic and individualized care and attention.
Nursing administration: Nursing administrators in their management of staff patients and facilities will have to ensure greater involvement in the assessment of patients and staff. Thereby devising and implementing plans to assist nurses in receiving the desired competencies required to provide individualized care to TB patients. Additionally, the nursing administration will have to develop and implement policies, protocols, and guidelines to enhance the individualized care and support provided to TB patients to increase compliance.
Nursing research: Research is essential to providing evidence for nursing practice, and this study has provided evidence for future investigative work. These findings are the sparks that will light the path for the execution of a more in-depth examination of “the factors influencing knowledge on the completion of treatment among TB patients under DOTS”, and further enhance nursing practice.
Ultimately however it is clear that the health facility of interest was able to retain all its clients on the DOTS program irrespective of their demographic, socioeconomic, or clinical characteristics. Interestingly clients registered concerns with meeting scheduled appointments, stigma, and food supplies. However, this could be explained by more than half being unemployed and having no annual income.
These issues will require further in-depth exploration with a larger sample size, more facilities, and a qualitative approach as this methodology only affords to provide a snapshot into the current scenario unique to this study population. Nonetheless, the information provided does reassure that the facility is maintaining the required standard of care and points out gaps requiring attention.
Nursing administrators in their management of staff patients and facilities will have to ensure greater involvement in the assessment of patients and staff. Thereby devising and implementing plans to assist nurses in receiving the desired competencies required to provide individualized care to TB patients. Additionally, the nursing administration will have to develop and implement policies, protocols, and guidelines to enhance the individualized care and support provided to TB patients to increase compliance.
The limitation of the study
The small sample size of 40 has limited generalization of the results as it relates to the Bahamas New Providence.
The data, collected in Bahamas New Providence, cannot necessarily be generalized to the wider Caribbean to make a generalized assumption about factors influencing knowledge on the completion of treatment among tuberculosis patients under the Directly Observed Treatment Strategy (DOTS).
Ethics approval
The UWI Campus Research Ethics Committee vide Ref no: CREC-SA.0476/08/202020. The UWI Ethics Committee located in Nassau, The Bahamas, Secretary and Director of Nursing at the Ministry of Public Health, Nassau, The Bahamas, written informed consent was obtained from the participants of the study.
Funding
This was a self-financed project. The authors received no external funds.
Author contributions
Esther S. Daniel: Conceptualization, Data Curation, Methodology, Formal Analysis,
Esther S. Daniel, Latasha Collie, Alice Neymour, Nicole K.A Martin-Chen, Kevin Moss, Virginia M. Victor, Kathy-Ann Lootawan: Writing-Original draft, Writing – review, and final editing. All authors read and approved the final manuscript.
Availability of data and materials
Available upon request by the 1st author (Dr. Esther S. Daniel)
Transparency declaration
The lead author (Dr. Esther Daniel) affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
- Tuberculosis (TB). World Health Organization.2024 Mar 20. https://www.who.int/news-room/fact-sheets/detail/tuberculosis
- Ministry of Health. Tuberculosis (TB) Control. Nassau: Ministry of Health; n.d. 2020 Feb 29. https://www.bahamas.gov.bs/wps/portal/public/HealthInitiatives/Tuberculosis control
- World Health Organization (WHO) 2016a Global Tuberculosis report. 2016 Geneva. WHO Bloom BR. Tuberculosis. Major Infectious Diseases. 3rd edition. U.S. National Library of Medicine; 2017 [cited 2020 Feb 22]. https://www.ncbi.nlm.gov/books/NBK525174
- HIV and Tuberculosis (TB) Understanding HIV/AIDS. National Institutes of Health. U.S. Department of Health and Human Services; 2019 [cited 2020Feb 11]. https://aidsinfo.nih.gov/understanding-hiv-aids/fact-sheets/26/90/hiv-and-tuberculosis--tb-/
- Seung KJ, Keshavjee S, Rich ML. Multidrug-Resistant Tuberculosis and Extensively Drug-Resistant Tuberculosis. Cold Spring Harb Perspect Med. 2015 Apr 27;5(9):a017863. doi: 10.1101/cshperspect.a017863. PMID: 25918181; PMCID: PMC4561400.
- Substance Abuse and Mental Health Services Administration (US). Health Care Systems and Substance Use Disorders. Facing Addiction in America: The Surgeon General's Report on Alcohol, Drugs, and Health. U.S. National Library of Medicine; [cited 2020, Mar 20]. https://www.ncbi.nlm.nih.gov/books/NBK424848/
- Yao X, Liu Y, Liu Y, Liu W, Ye Z, Zheng C, Ge S. Multiplex analysis of plasma cytokines/chemokines showing different immune responses in active TB patients, latent TB infection and healthy participants. Tuberculosis (Edinb). 2017 Dec; 107:88-94. doi: 10.1016/j.tube.2017.07.013. Epub 2017 Aug 3. PMID: 29050777.
- Herrero MB, Ramos S, Arrossi S. Determinants of non adherence to tuberculosis treatment in Argentina: barriers related to access to treatment. Rev Bras Epidemiol. 2015 Apr-Jun;18(2):287-98. doi: 10.1590/1980-5497201500020001. PMID: 26083503.
- Mwanza J. Sickrole Compliance and Sickrole Deviance among Tuberculosis Patients on Treatment in Kanyama, a Zambian Shanty Compound. Adv. Appl. Sociol. 2016 [cited 2020 Mar 15];6(01). https://www.scirp.org/journal/paperinformation.aspx?paperid=62834
- Kaona FA, Tuba M, Siziya S, Sikaona L. An assessment of factors contributing to treatment adherence and knowledge of TB transmission among patients on TB treatment. BMC Public Health. 2004 Dec 29;4:68. doi: 10.1186/1471-2458-4-68. PMID: 15625004; PMCID: PMC545081.
- Sanneh AF, Pollock JI. Comparison of Pulmonary TB DOTS clinic medication before and after the introduction of daily DOTS treatment and attitudes of treatment defaulters in the Western Division of the Gambia. Afr Health Sci. 2010 Jun;10(2):165-71. PMID: 21326970; PMCID: PMC2956295.
- Bam TS, Gunneberg C, Chamroonsawasdi K, Bam DS, Aalberg O, Kasland O, Shiyalap K, Srisorrachatr S. Factors affecting patient adherence to DOTS in urban Kathmandu, Nepal. Int J Tuberc Lung Dis. 2006 Mar;10(3):270-6. PMID: 16562706.
- Mushtaq MU, Shahid U, Abdullah HM, Saeed A, Omer F, Shad MA, Siddiqui AM, Akram J. Urban-rural inequities in knowledge, attitudes and practices regarding tuberculosis in two districts of Pakistan's Punjab province. Int J Equity Health. 2011 Feb 4;10:8. doi: 10.1186/1475-9276-10-8. PMID: 21294873; PMCID: PMC3045313.
- Wang J, Fei Y, Shen H, Xu B. Gender difference in knowledge of tuberculosis and associated health-care seeking behaviors: a cross-sectional study in a rural area of China. BMC Public Health. 2008 Oct 8;8:354. doi: 10.1186/1471-2458-8-354. PMID: 18842127; PMCID: PMC2577657.
- McIntosh J, Forbes N, Moss K, Frankson MA. 1373. Clinical Presentation, Demographics, and Outcomes of Cases of Tuberculosis (TB) at Princess Margaret Hospital, Nassau, The Bahamas 2014–2016. In Open Forum Infectious Diseases 2019 Oct (Vol. 6, No. Suppl 2, p. S498). Oxford University Press.
- Reumers L, Bekker M, Hilderink H, Jansen M, Helderman JK, Ruwaard D. Qualitative modelling of social determinants of health using group model building: the case of debt, poverty, and health. Int J Equity Health. 2022 May 19;21(1):72. doi: 10.1186/s12939-022-01676-7. PMID: 35590354; PMCID: PMC9118602.
- Nedjat S, Mehrdad R, Yunesian M, Pouragha H, Biagi V, Monazzam-Esmaeelpour MR. Prospective cohort study on the social determinants of health: Tehran University of Medical Sciences employees` cohort (TEC) study protocol. BMC Public Health. 2020 Nov 13;20(1):1703. doi: 10.1186/s12889-020-09798-9. PMID: 33187513; PMCID: PMC7666496.
- World Health Organization (WHO). Global tuberculosis report. Geneva, Switzerland: World Health Organization. 2019.
- Tola HH, Tol A, Shojaeizadeh D, Garmaroudi G. Tuberculosis Treatment Non-Adherence and Lost to Follow Up among TB Patients with or without HIV in Developing Countries: A Systematic Review. Iran J Public Health. 2015 Jan;44(1):1-11. PMID: 26060770; PMCID: PMC4449995.
- Adjemian J, Frankland TB, Daida YG, Honda JR, Olivier KN, Zelazny A, Honda S, Prevots DR. Epidemiology of Nontuberculous Mycobacterial Lung Disease and Tuberculosis, Hawaii, USA. Emerg Infect Dis. 2017 Mar;23(3):439-447. doi: 10.3201/eid2303.161827. PMID: 28221128; PMCID: PMC5382761.
- Phelan J, Coll F, McNerney R, Ascher DB, Pires DE, Furnham N, Coeck N, Hill-Cawthorne GA, Nair MB, Mallard K, Ramsay A, Campino S, Hibberd ML, Pain A, Rigouts L, Clark TG. Mycobacterium tuberculosis whole genome sequencing and protein structure modelling provides insights into anti-tuberculosis drug resistance. BMC Med. 2016 Mar 23;14:31. doi: 10.1186/s12916-016-0575-9. PMID: 27005572; PMCID: PMC4804620.
- Bloom BR, Atun R, Cohen T, Dye C, Fraser H, Gomez GB, et al. Chapter 11 Tuberculosis. In Holmes KK, Bertozzi S, Bloom BR, editors. Major infectious diseases. 3rd ed. Washington, DC: The World Bank; 2017 [cited 2020 Feb 22]. Chapter 11. https://www.ncbi.nlm.nih.gov/books/NBK525174/