More Information
Submitted: November 09, 2023 | Approved: November 20, 2023 | Published: November 21, 2023
How to cite this article: Sandhu SS, Mallavarapu S, Smith SM, Garcia MM. Strategies to Prevent Lower-Extremity Positioning Injuries During Long-Duration Surgery in the Lithotomy Position: Our Techniques and Clinical Outcomes Following Genital Gender-Affirming Surgeries. Clin J Nurs Care Pract. 2023; 7: 015-024.
DOI: 10.29328/journal.cjncp.1001047
Copyright License: © 2023 Sandhu SS, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Gender change surgery; Description; Position; Leg injury; Leg injuries; Compartment syndrome; Paresthesia; Injury; Nervous system; Pressure ulcer; Rhabdomyolysis
Strategies to Prevent Lower-Extremity Positioning Injuries During Long-Duration Surgery in the Lithotomy Position: Our Techniques and Clinical Outcomes Following Genital Gender-Affirming Surgeries
Sandeep S Sandhu1,2, Samhita Mallavarapu1,2, Shannon M Smith1,2 and Maurice M Garcia1,2*
1Department of Urology, Cedars-Sinai Medical Center, Los Angeles, California, USA
2Cedars-Sinai Transgender Surgery and Health Program, Los Angeles, California, USA
*Address for Correspondence: Maurice M Garcia, MD, MAS, Department of Urology, 8631 W. Third Street, Suite 420E, Los Angeles, CA, 90048, USA Email: [email protected]
Purpose: Lower-extremity (LE) injuries due to prolonged surgery duration in the dorsal lithotomy (DL) position are often morbid and can significantly affect the patient’s short and long-term quality of life. These include the development of lower extremity pressure ulcers, neuropathies, rhabdomyolysis, and compartment syndromes. As compared to other surgeries, this risk is increased in patients undergoing genital gender-affirming surgery (gGAS) due to the relatively long operative time of these surgeries related to their high complexity. Our study aimed to describe our technique for preventing LE injuries in the DL position, and to evaluate our positioning-related post-operative complications and rates.
Materials and Methods: We describe our technique for positioning in the dorsal lithotomy position, with an emphasis on injury prevention. We ensure a specific padding technique of the LE, we alert surgical assistants to not lean/rest on the LE, and we schedule LE checks and repositioning throughout the case to prevent and mitigate occult injuries.
Herein, we report our clinical positioning-related outcomes and complications among all patients undergoing gGAS procedures lasting >300 minutes between January 2017 to March 2023.
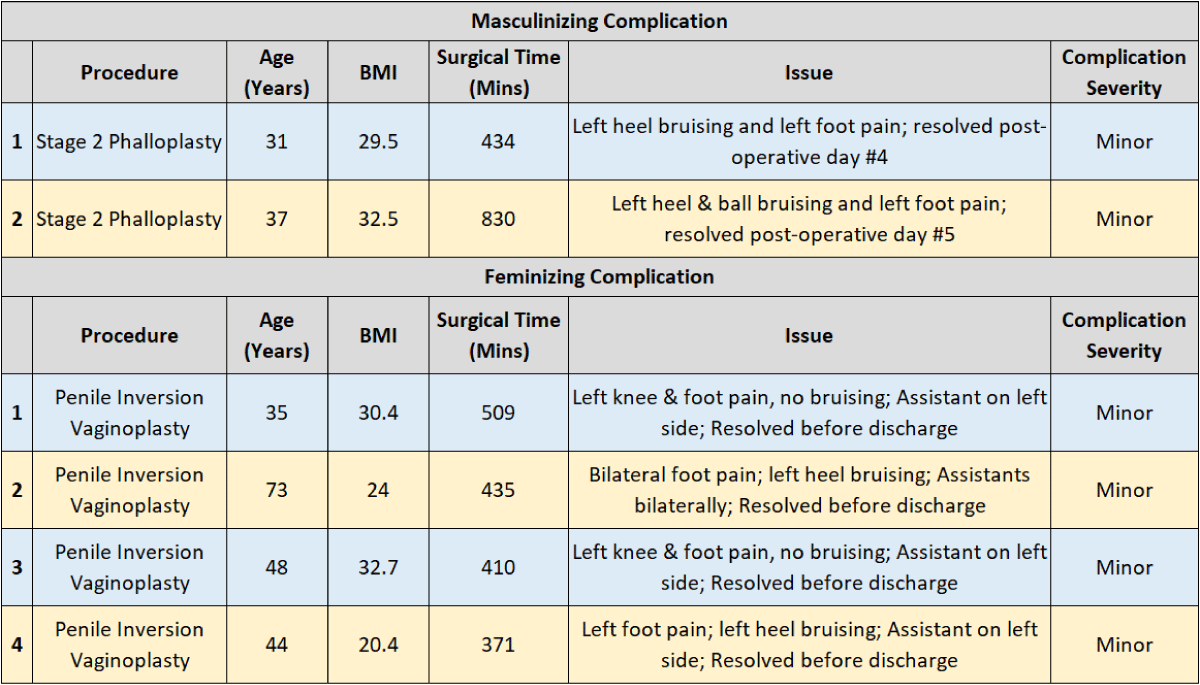
Results: A total of 227 patients underwent 310 surgical procedures (156 masculinizing, 154 feminizing gGAS procedures). Mean operative time was 495.5 minutes+/-156.5 minutes (SD) (Range 300–1095 minutes). A total of 6/227 (2.6%) patients (2 masculinizing and 4 feminizing surgical patients) had transient, self-limited LE pain post-op. No (0%) patients had major complications including chronic nerve injury, pressure ulcers, rhabdomyolysis, or compartment syndrome.
Conclusions: Our study is the first to describe a replicable technique, and specifically which integrates the OR team and nursing staff, to prevent LE injuries during DL. We show that it is possible to achieve a 0%-to-rare incidence of major LE injury during long-duration surgeries.
Patient positioning at the time of surgery plays a critical role in determining outcomes. Urologists, Obstetricians Gynaecologist and General and Plastic Surgeons commonly place patients in the lithotomy position to expose the pelvis and perineum [1-9]. This position provides excellent access to the perineum and affords placement of an assistant between the patient’s legs during intra-abdominal surgery.
Prior studies assessing lower extremity (LE) injuries secondary to dorsal lithotomy (DL) positioning consistently cite only causative pathophysiologic factors to explain the injury. They also cite position duration as a principal risk factor for injury [10]. Positioning injuries can significantly adversely affect both patients and the healthcare system through acute care requirements, chronic rehabilitation, and potential malpractice litigation [11,12].
Genital gender-affirming surgeries (gGAS) are complex and typically of long (> 5 hours) duration. Surgeons who perform these and other similarly long procedures should be aware that LE injuries are more likely to occur than in shorter cases. Because LE positioning injuries are so morbid and associated with such high costs, it is important for surgeons to understand the pathophysiology of LE injuries, and techniques and practices to altogether prevent injuries, to reduce complication rates [9,13,14].
The purpose of this study is to I. Review the pathophysiology of injuries to the LE during DL positioning; II. Review key findings from the literature about how LE positioning injuries can be avoided; III. Describe our positioning technique and peri-operative injury prevention strategies; and IV. Review the incidence of DL LE positioning injuries from our own institution for all gGAS surgeries of > 5 hours over a 6-year period.
We performed a literature review using PubMed. Keywords included “dorsal lithotomy”, “lower extremity” and “injury”, and articles published between 1994 to 2023 were reviewed. Articles describing the pathophysiology of LE injuries during DL positioning, specifically, pressure injuries, neuropathies, rhabdomyolysis, and compartment syndrome were reviewed. We summarized from the literature specific pathophysiologic processes that cause LE positioning injuries, and the correlate recommendations to prevent the resulting injuries.
A chart review was undertaken for all patients undergoing gGAS from January 2017 to March 2023. We included surgeries lasting longer than 5 hours (300 minutes) duration. Complications were reviewed and categorized into “minor” and “major” complications. Minor complications were defined as those complications that required no additional intervention and resolved spontaneously prior to discharge from the hospital. Major complications were defined as complications that required additional medical or surgical intervention, or that persisted after the patient was discharged from the hospital. These included compartment syndromes (CS), acute or chronic LE neuropathies, pressure ulcers, or rhabdomyolysis.
Literature review: Pathophysiology of LE injuries in the DL position
The most common LE injuries secondary to DL positioning are pressure ulcers, neuropathies, rhabdomyolysis, and LE CS [9,14-17]. The pathophysiology and associated risk factors vary depending on the type of injury and are described below.
Pressure ulcers: Pressure ulcers are caused by localized pressure and shear forces to the skin and underlying tissues that contain vascular support, commonly over bony prominences. The resulting ischemia leads to tissue breakdown, with injuries sometimes presenting long after the initial insult [14].
Risk factors include surgical positioning where weight support is focused on small surface areas, and duration of uninterrupted compression [14]. Body mass index (BMI) extremes also increase this risk compared to people with normal body habitus. Low BMI (< 20 kg/m2) individuals are at elevated risk due to limited subcutaneous tissue causing compression against bony prominences, while high BMI (> 30 kg/m2) individuals are at increased risk due to increasing pressure loads [14,18]. Other risk factors include patients with an impaired cardiovascular system, including a history of diabetes mellitus, peripheral vascular disease, and smoking status. Finally, neurologic and physical insults impairing mobility, increased age > 70 years, dehydration, nutritional deficiencies, and hypothermia also increase the risk of developing pressure ulcers [14].
Neuropathies: The incidence of postoperative lower-extremity neuropathy following DL is reported to be 0.6% - 1.2% [14,17]. These occur due to a combination of stretch, compression, and ischemia-induced nerve injuries. [9,14,17,19]. Neuropathies of the LE most commonly affect the common peroneal nerve (78%), sciatic nerve (15%), and femoral nerves (7%) [20]. Peroneal nerve injuries are due to compression against the fibular head, typically from mal-positioning of the LE in an Allen or “candy-cane” stirrup) resulting in impaired sensation on the lateral aspect of the calf and dorsum of the foot, and/or a foot drop due to impaired ankle dorsiflexion. Sciatic nerve injuries occur due to extreme hip flexion (> 90°) and hyperextension of the knee. Patients with sciatic neuropathy will complain of impaired sensation on the posterior aspect of their leg, and difficulties with knee flexion and ankle dorsiflexion. Femoral nerve injuries occur due to extreme hip abduction and/or extreme hip flexion with external rotation, which causes compression of the femoral nerve against the inguinal ligament. Clinical presentation of femoral neuropathy include deficient (during normal activity) hip flexion and knee extension, often in combination with a reduced patellar reflex [9,14,17].
Dorsal lithotomy LE neuropathies can develop due to incorrect positioning, or with prolonged surgery duration. Additional risk factors include conditions that impair the circulatory system, such as diabetes mellitus, peripheral vascular disease, smoking (including tobacco, marijuana, and vaping), pre-existing neuropathies, other acute and chronic conditions that limit physical mobility, and lastly, advanced age > 70 years [2,10,14,17,21-23].
Rhabdomyolysis: Rhabdomyolysis related to DL positioning occurs due to direct LE-muscle injury and/or ischemic injury to muscle myocytes, which leads to tissue necrosis, and elevated creatinine kinase level, with resulting acute renal injury with myoglobinuria [16]. An initial insult to the muscle causes a cyclical pathway resulting in a release of sodium and calcium ions from the sarcoplasmic reticulum of the muscle which is taken up by surrounding myocytes, resulting in sustained myofibrillar contraction, cellular swelling secondary to indrawing of water, and depletion of adenosine triphosphate (ATP). The resulting injury and myocyte breakdown lead to an inflammatory process causing further tissue damage [16]. Specific surgical risk factors include prolonged surgery duration, muscle compression from DL-positioning, and muscle ischemia from DL-positioning (e.g. prolonged maintenance of the LE above heart level; foot dorsiflexion) [9,14].
Compartment syndrome: Compartment syndrome (CS) is a rare but dreaded surgical complication, occurring with an incidence that ranges from 1:3500 to 1:8720 cases of patients where the patient is in the DL position [24,25]. While CS most commonly occurs in the LE, gluteal CS does occur, with an incidence of 3% to 11% of all cases of CS [26]. Cases of bilateral LE CS have been reported even after 90-minute procedures in the DL position [9]. CS is believed to occur due to decreased muscle perfusion pressure, coupled with increasing compartment pressures (secondary to ischemic tissue swelling) within a fixed-volume compartment, which in a vicious cycle further impairs tissue perfusion, and results in further tissue ischemia, necrosis, and swelling. Management of this urgent condition requires emergency fasciotomy to relieve the pressure and prevent further injury [15]. Sequelae of compartment syndrome can include permanent loss of motor function, and possibly, need for amputation [3,24,27-29].
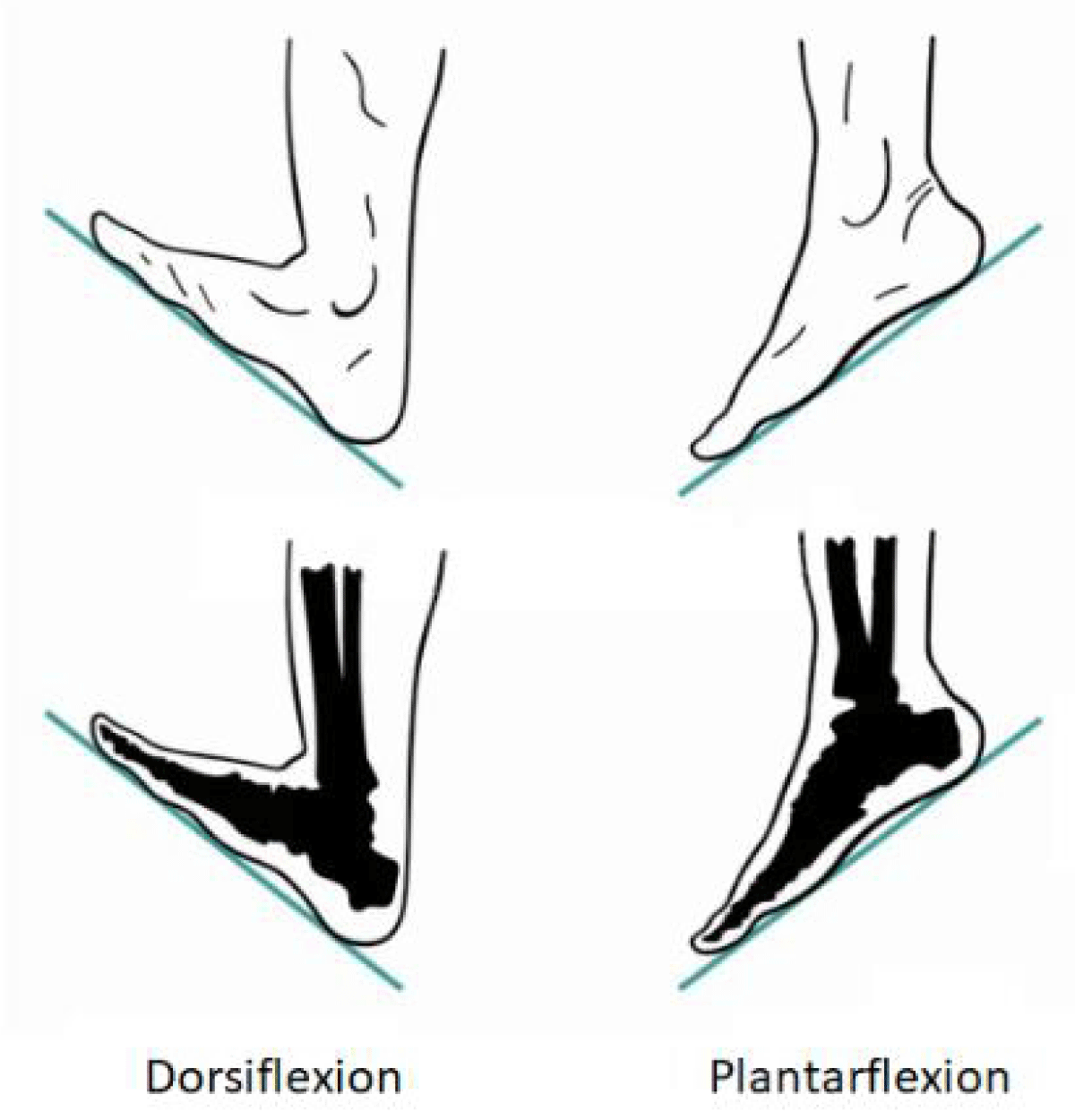
Risk factors for LE CS include extended duration of surgery, and mal-positioning of the leg inside LE supports that cause external compression of the LE muscle compartments [9,14,15]. Another risk factor is the dorsi-flexed positioning of the foot inside LE supports. Foot dorsiflexion increases posterior compartment pressures (Figure 1) and injury risk, while plantar flexion decreases resting calf posterior compartment pressures, thereby reducing injury risk [4,25]. Finally, positions where the LE is raised above the level of the heart for extended periods of time reduce muscle perfusion and increase the risk of ischemia-induced soft-tissue injury and swelling, which increases the risk of LE CS [9,25].
Figure 1: Ankle dorsi vs. plantarflexion
Literature review: Recommended strategies for the prevention of LE injuries in the DL position
The Association of Perioperative Registered Nurses (AORN) provides guidance for safe positioning during DL to prevent LE injuries [9,14]. These recommendations include appropriate positioning in LE supports. Both legs should be placed into supports simultaneously and in a controlled manner. Both legs should rest at an even height, with weight support over a large surface area, to prevent injury. Both legs should also be removed from the LE supports in a simultaneous fashion [9].
AORN also recommends the LEs be positioned with focused attention to prevent nerve injuries to the femoral, sciatic, and common peroneal nerves. This includes avoiding extreme flexion or extension of the hips and knees and avoiding extreme abduction and external rotation of the hips. To ensure adequate LE tissue perfusion, the LEs should be in line or below the level of the heart, and ideally, the patient’s heels should be in the lowest position possible. Another AORN recommendation is that personnel scrubbed into the case do not lean against or rest any part of their body upon the patient’s LE, and, that the LEs be adequately protected with padding to prevent compression of the LE against the leg supports [9].
AORN recognizes that prolonged surgery duration, and prolonged uninterrupted positioning in higher risk positions (e.g., high-lithotomy; feet positioned above the level of the heart, Trendelenburg, and ankle dorsi-flexed positions) all contribute to DL-positioning related injuries [9,25]. AORN recommends placing the patient in the DL position for as short a duration as possible, and that the legs be repositioned to a neutral, heart-level position, at established intervals throughout prolonged surgeries. Similarly, whenever a patient is placed into high-lithotomy, the legs should be brought down during regularly timed breaks in order to allow for LE reperfusion. [9]. The feet should be slightly plantarflexed relative to the leg, to reduce pressure in the posterior muscle compartments [4,25]. In addition, AORN recommends that to reduce the risk of CS-related rhabdomyolysis, a neutral urine pH be maintained, and when regional anesthesia is used, that motor blockade be avoided [25].
Description of our genital GAS surgery program clinical outcomes assessment, LE positioning technique and peri-operative injury prevention strategies
We conducted a retrospective chart review of all patients at our institution who underwent masculinizing and feminizing gGAS in the DL position with surgery duration greater than 5 hours (300 minutes), from January 2017 to March 2023. Cases that lasted less than 5 hours in DL were excluded. All patients were placed in the DL position for the entirety of their surgical procedure, with the exception of patients who underwent radial-artery forearm free-flap phallourethroplasty, who are normally positioned in a prone position for ~1.5 hrs at the start of their case (to undergo harvest of intergluteal full-thickness skin grafts to cover the arm donor-site), before they are re-positioned to the DL position for the remaining ~8 hours of the phallourethroplasty surgery.
Primary endpoints included LE complications including self-limiting musculoskeletal injuries, femoral nerve, sciatic nerve, and common peroneal nerve injuries, development of pressure ulcers of the sacrum and heel, development of rhabdomyolysis, and, development of compartment syndrome requiring fasciotomy.
Our technique for perioperative positioning of the lower limbs: All patients included in this study were placed in the DL position with their LEs in AllenTM stirrups during their surgery. For patients who underwent harvest of a radial-artery forearm flap, standard-length (yellow) AllenTM stirrups were used, while for patients undergoing flap-harvest from the anterior lateral thigh (ALT), we always use the shorter blue-colored AllenTM stirrups, which differ from the yellow stirrups in that their long lateral segment that supports the calf is shorter. We use these when harvesting a flap from the thigh because the shorter length of the long segment supporting the calf affords the surgeon greater access to the anterior thigh flap harvest site.
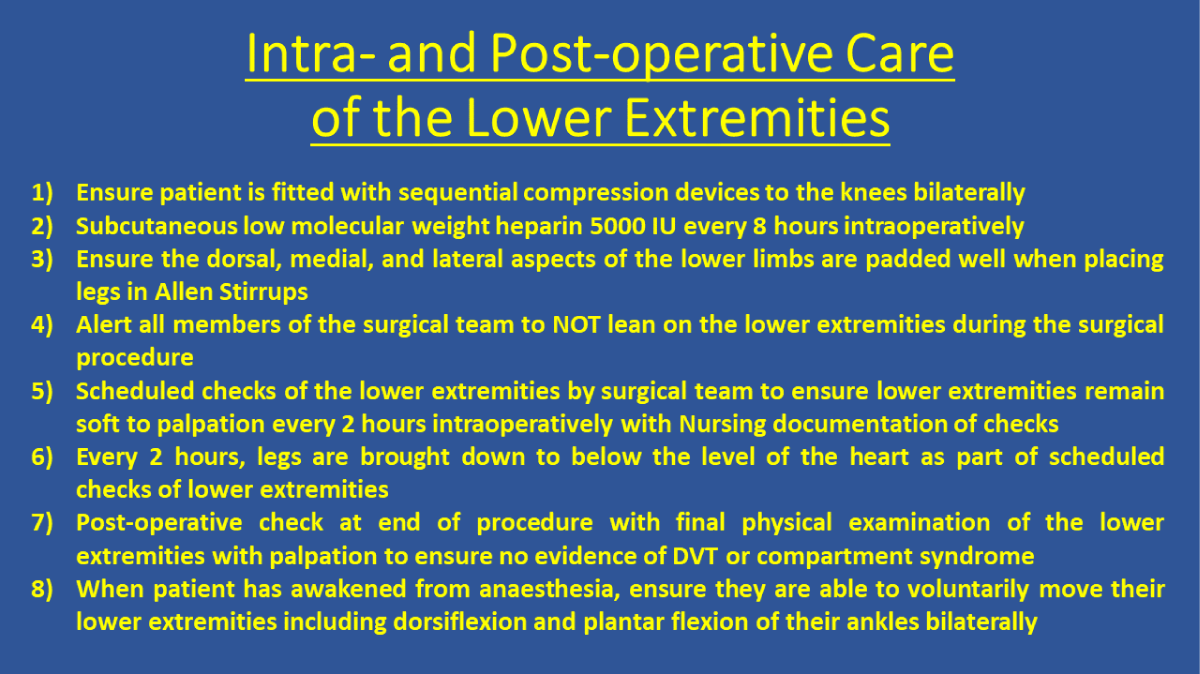
Given the long duration of the procedures assessed, we undertake standardized intra-operative precautions to minimize the risk of LE injuries as recommended by AORN (Figure 2). [9]. For example, all patients are fitted with sequential compression devices (SCD) below the knee and all patients receive subcutaneous low molecular weight heparin every 8 hours for prophylactic prevention of venous thromboembolic events during surgery. Also, every 2 hours we visually inspect the LEs (we use see-through leggings), and manually inspect (by palpating the calves and thighs to assess for swelling or firmness suggestive of compartment syndrome) every 2 hours. During these regularly scheduled checks, the LEs are lowered below the level of the heart to promote reperfusion of tissues rendered ischemic from positioning. Lastly, during these checks, we also confirmed among all surgeons in attendance that no one was compressing the LEs by leaning or resting their bodies on them.
Figure 2: Our program’s Intra-operative and Post-operative Care of the Lower Extremities poster.
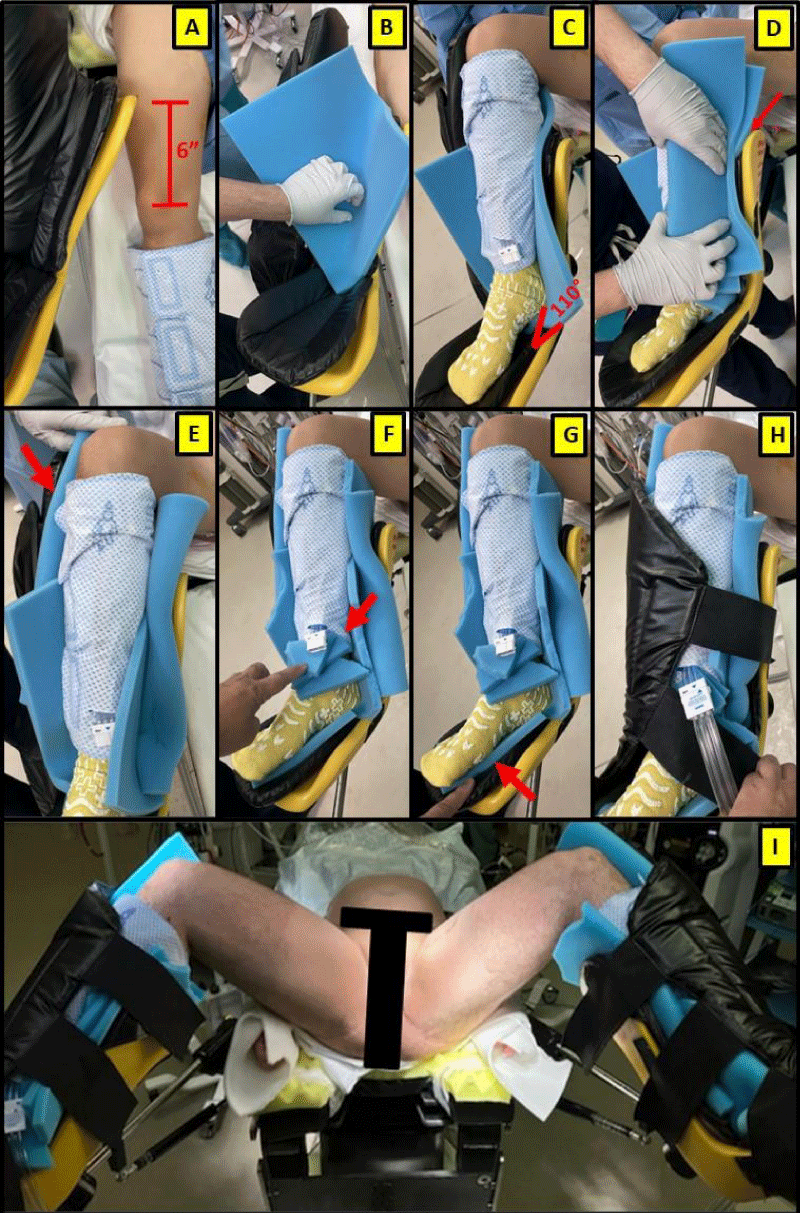
Intra-operative patient positioning: Following induction of general anesthesia and securing the endotracheal tube, patients are positioned so their sacrum is resting superior to the body padding, reducing the risk of lumbosacral injuries. The measures outlined below are taken to protect the LE’s from injury (Figure 3).
Figure 3: Technique for ensuring safe lower extremities positioning (consent for use of intraoperative photography obtained from the patient).
After induction and with the patient in a supine position, we begin by first repositioning the patient on the table to ensure that their perineum is at the edge of the table, as desired. Next, the AllenTM stirrups are affixed to the surgery table. We have found that to ensure that the angle of knee flexion is slightly greater than 90 degrees, we position the Allen-stirrup unit so that the cephalad-end of the medial aspect of the stirrup-boot is approximately 6-inches cephalad to the ipsilateral patella. This facilitates secure placement of the patient’s heel within the boot to prevent compression of the popliteal fossa.
To support the LE inside the AllenTM stirrup we use three pieces of ½-inch-thick foam padding to protect each lower leg. The first piece of foam is laid flat in the heel and calf-support areas within the boot before each leg is placed into the stirrup. The foot should be slightly plantarflexed (Figure 1) to minimize resting LE posterior-compartment pressure. We also confirm that there is no compression upon the popliteal fossa. We then place an additional piece of foam, folded lengthwise, between both the medial and lateral aspects of the lower leg and stirrup boot (this adds a 1-inch total thickness of foam support on both sides of each leg). This extra padding reduces the risk of direct compression, most importantly around the fibula head, where the risk of a common peroneal nerve injury is greatest. The additional foam above the medial aspect of the stirrup is cut and a piece is placed under the connection point for the SCD tubing, and the remaining piece of foam is placed under the sole of the patient’s foot. After ensuring all potential compressive areas are protected, the patient’s leg is then loosely secured within the Allen stirrup using the Velcro straps to prevent ventral compression.
Because we routinely use SCDs, to prevent ischemia-induing compression injury to the LEs we take care to ensure that the SCD tubing does not cross the midline of the lower leg, and, that the hard-plastic connector piece that connects the tubing to the SCD lays flat (never perpendicular to) the leg. To further protect the leg from the SCD connector we always place small torn pieces of foam between the leg and the connector piece.
After the legs are positioned into the Allen TMTM stirrups, the legs are then positioned with the knees flexed at ~110 degrees, and to allow the surgeon and assistants access to the perineum, the hips externally rotated ~45 degrees.
Review the incidence of DL LE positioning injuries from our own institution for all gGAS surgeries of > 5 hours duration over a 6-year period
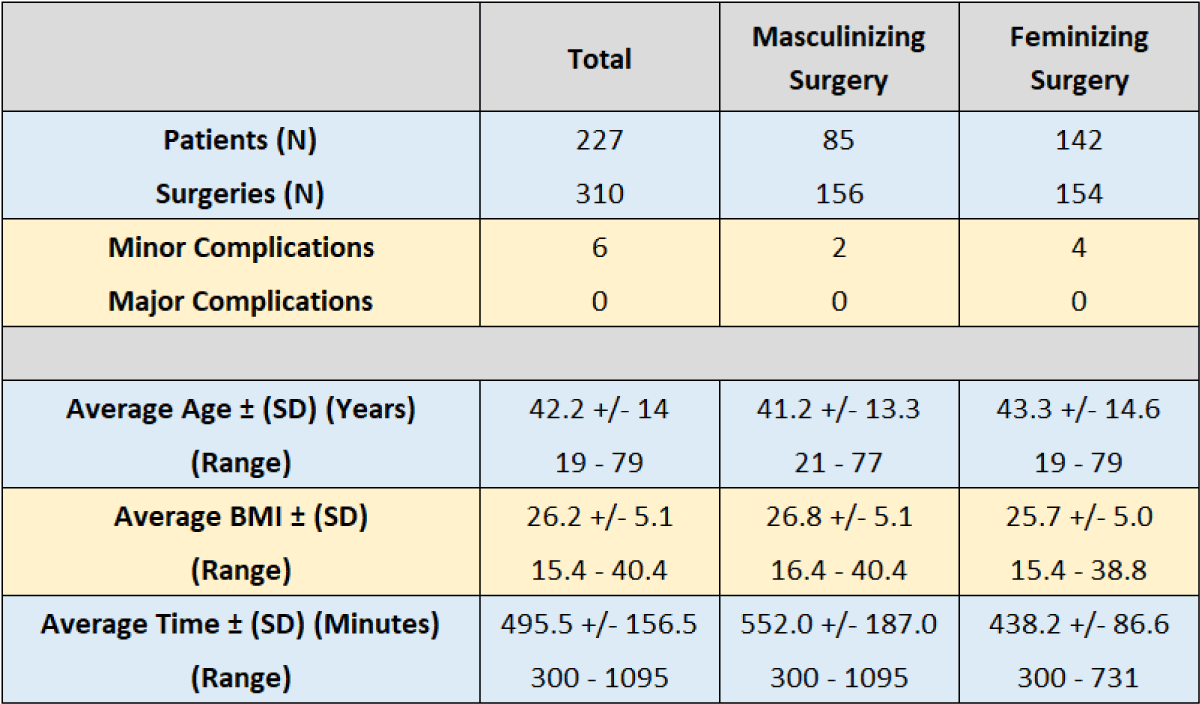
A total of 227 patients who underwent gGAS from our institution’s Transgender Health and Surgery Program were included in this study. Of these, 85 individuals underwent 156 masculinizing gGAS procedures, and 142 individuals underwent 154 feminizing gGAS procedures.
Demographic information is included in Table 1, and specific complications for both masculinizing and feminizing surgical procedures are described in Table 2.
Table 1: Demographic information for patients undergoing gGAS, and mean surgical durations.
Table 2: Procedures and associated complications for patients undergoing gGAS.
Overall, a total of 6 (2.6%) patients suffered short-term, minor complications related to the pain of the foot or knee (Table 2), which we classified as “minor” because none required operative intervention and resolved prior to discharge from the hospital. Zero (0%) patients suffered chronic or significant complications such as compartment syndrome, acute or chronic nerve injury, pressure ulcers, or rhabdomyolysis.
Genital GAS is a rapidly growing field. The practice of gGAS is reported to have increased 152-fold from 2010-2018 [13]. Because gGAS surgeries are complex, typically of long duration, and performed in the DL position, it is important that surgeons and OR nursing staff understand how LE injuries occur, and, how to prevent them. Furthermore, because advanced minimally invasive surgical techniques using laparoscopic and robot-assisted lap gGAS techniques typically require both DL and steep Trendelenburg positioning, it is essential that surgeons and OR teams also be aware of strategies to prevent DL-related positioning injuries during these procedures [2,5-7,30,31].
Poor patient positioning can have devastating short and long-term consequences including soft-tissue injuries, loss of function to the affected limb, or amputation of the affected limb [4,7,9,10,21,32]. Because positioning injuries are rare, and, to a seemingly great degree preventable, the standard in the future may be to classify them as “never events”, on par with falls, CAUTI, and similar adverse events for which there is prevention data. Across our 310 surgical cases, each of > 5 hours duration (mean: 8.25 hours), our LE positioning practices have yielded a total of 6/310 (1.9%) minor LE injuries that were all self-limited and did not require intervention. No patient (0%) sustained a severe injury (i.e., requiring operative intervention), or that was associated with chronic deficits or sequelae.
Patients in our series who suffered LE complications varied in age and BMI, showing that even young, healthy patients are at risk of LE injuries during long-duration surgeries. This suggests that injury prevention strategies should be implemented universally as a standard of care. In the United States, 69% of the population is overweight or obese, and 36% of the population is classed as obese [33]. Familiarity with Injury prevention strategies is especially important as the U.S. population’s mean BMI increases and as the mean age at surgery and the presence of a greater number of comorbidities at the time of surgery increase. Many gGAS surgeons have BMI limit criteria for patients seeking gGAS (e.g. BMI < 30) in an attempt to reduce the risk of peri-operative complications associated with obesity [34].
A study of our own practices and patient outcomes has taught us that a common mechanism for LE injuries is from surgery assistants (who typically stand beside the patient while the primary surgeon is seated at the perineum) unwittingly leaning on or resting a hand upon the patient during surgery [25]. Fortunately, this can easily be prevented by the primary surgeon when the latter announces that these precautions be followed by all of their assistants, and then, when the surgeon monitors their team’s actions throughout the surgery. Our work has also taught us that a systematic approach to the prevention of LE injury requires active surgeon and nurse participation. This approach begins with the surgeon integrating routine leg and positioning checks into the standard OR-wide “Time Out” at the beginning of the surgery. This way, surgeons, anesthesia, and nursing teams are made aware of the increased risk for LE DL injuries, and, become responsible for ensuring that the LEs are checked at timed intervals throughout the surgery (Figure 2). Routine scheduled visual inspection of the legs with transparent leg covers, and routine palpation for firmness and swelling of the legs certainly do not guarantee injury prevention or detection, but, they help ensure awareness among staff, and possibly, early detection of any injury that may have already occurred. Routine scheduled “pauses” of LE elevation by momentarily lowering the legs so the feet are below the level of the heart facilitates examination of the LE, promotes tissue reperfusion, and at a minimum mitigates the degree of any injury that may have already started to occur.
Our practice of directing the routine assessment and re-positioning of the LEs by the nursing team into the surgical workflow as a “standard procedure” ensures that these interventions are actually performed. When only the surgeon is responsible for routine assessment and LE repositioning, these are often not performed because the surgeon “forgets” to do so owing to their attention being focused on other aspects of the surgery. Integration of positioning checks into the formal operating room workflow increases patient safety, and, because such assessments are documented in the medical record, these help serve as medico-legal protection for the surgeon and operating room staff by documenting attention to prevention of DL LE-related complications.
Many studies and guidelines have outlined the need for adequate padding when positioning patients, but, to our knowledge, no publications have specifically outlined their techniques and strategies to prevent LE injury during DL [3,10,12,35,36]. Our work is the first to do so. Many of the published studies outline the potential issues that can arise with poor positioning, and pre-operative steps which can help, but there is limited information related to specific peri-operative care guidance related to appropriate padding of the patient’s LEs to reduce injury risk [37,38].
Previous studies report that the risk of peripheral neuropathy associated with DL LE injury ranges from 0.03% to 47% [6,21,36,39,40]. These injuries have also been noted in the obstetrics literature, as women who are giving birth vaginally are often placed in an exaggerated lithotomy position. Lower-extremity nerve injuries in vaginal births occur at a rate of 0.3% to 1.8%. This shows that even during shorter procedures LE injuries can still occur, and so care must be taken to prevent these injuries [1,23]. Eighty percent of all LE neuropathies involve the common peroneal nerve from compression against the fibular head, leading to foot drop and loss of sensation over the lateral aspect of the calf and dorsum of the foot [12]. This occurs with extreme hip flexion and external rotation, so safe positioning of the LE at the time of surgery is critical to prevent injury.
Another devastating complication associated with prolonged surgery is compartment syndrome. LE-DL-associated CS occurs at a rate of 1:3500 to 1:8720 surgeries [24,25]. LE CS has significant ramifications: need for further urgent surgical intervention (e.g. primary fasciotomy, with reassessment under anesthesia), possible loss of the affected limb, development of rhabdomyolysis, acute multi-organ failure, and even death [4]. Other morbid sequelae include the need for prolonged rehabilitation, chronic neuro-muscular deficit, possible compromise to primary surgical outcomes, and the additional costs of all interventions and follow-up care to our healthcare system.
LE injuries can also result in medico-legal litigation and related costs to both patient and provider. The authors of this paper are aware of at least three LE-CS injuries that occurred with gGAS surgeries at outside institutions which have resulted in chronically debilitating injuries with long-term consequences for these patients, and, costly medico-legal litigation.
Multiple studies have described the etiology of LE CS [25,28,41,42]. The act of placing the LEs in the DL position immediately increased the resting compartment pressures as compared to the supine position [25,42]. They also noted a reduction in mean arterial pressure by 0.78mmHg for every centimeter the LE was raised above the level of the right atrium, and the act of placing the patient in a Trendelenburg position further reduced perfusion to the LEs [25,41] The positioning of the limbs also impacted compartment pressures with extreme knee and hip flexion, and ankle dorsiflexion increasing calf pressures [25,28]. Dorsi-flexion, combined with compression from sequential compression devices, can increase compartment pressures to critical levels during surgery, resulting in tissue ischemia and edema [25,43]. External pressures from surgical assistants leaning on the LE can have similar effects [25]. Finally, in the setting of an already established injury and elevated compartment pressures, the act of restoring perfusion by returning the LEs to a supine position at the end of a surgical case would increase the compartment pressures further, causing a reperfusion injury [25].
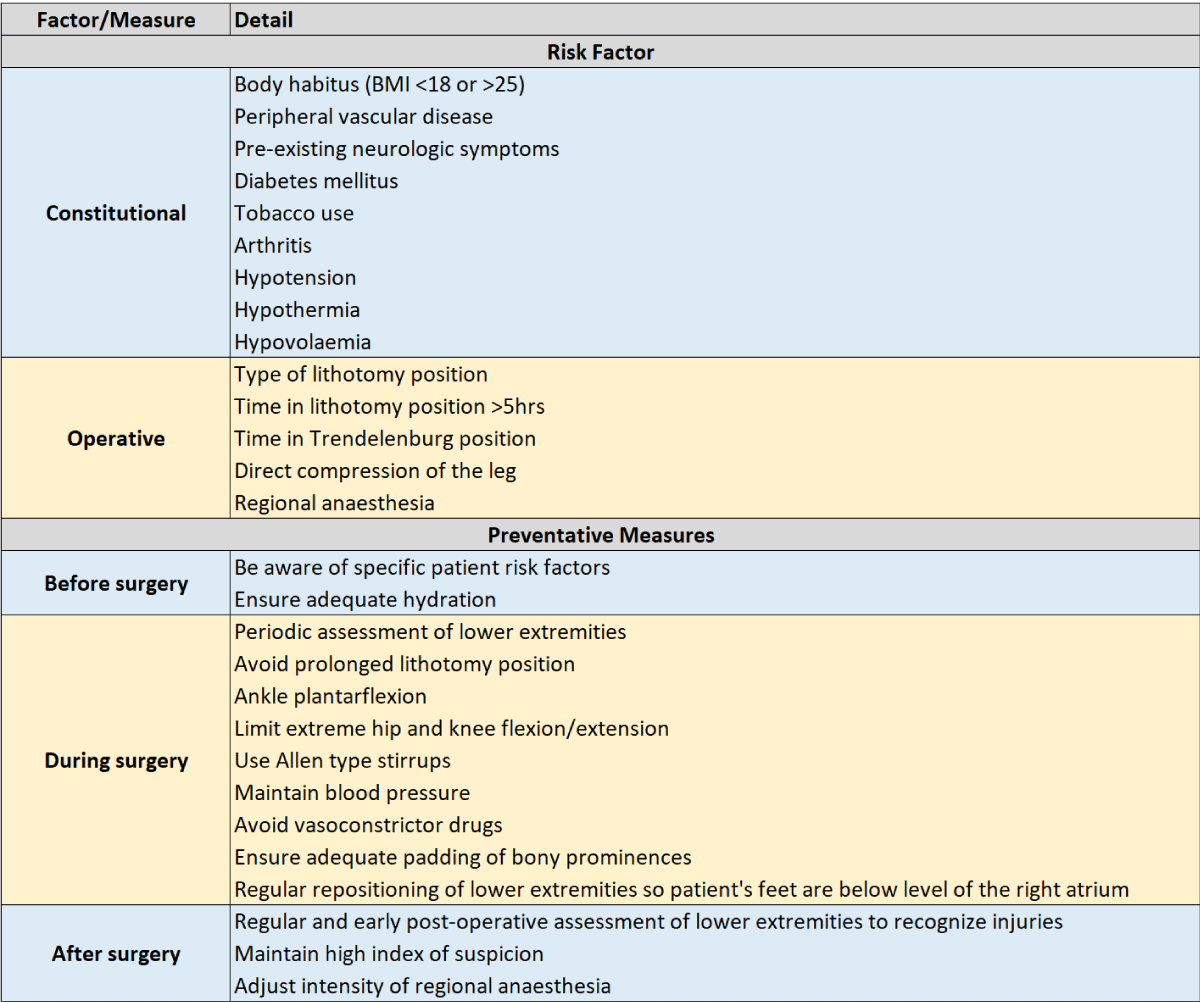
Several studies have outlined specific risk factors and preventative measures that can be undertaken by the surgical team to prevent LE CS [8,25,32]. Extremes in BMI (< 18 kg/m2 or > 25 kg/m2), vasculopathy, and impaired circulatory compromise related to hypothermia, hypotension, and hypovolaemia all predispose patients to an elevated risk of compartment syndrome [8,25,27]. In addition, operative factors such as prolonged lithotomy position for longer than 5 hours, direct vessel compression, and epidural analgesia with motor blockade can also increase the risk of developing compartment syndrome [9,25,29].
Cited studies also outline other preventative strategies, included in Table 3, which include: 1. Maintenance of adequate circulatory support pre and intra-operatively with adequate hydration, 2. Avoiding the use of vasoconstrictive medications when possible; 3. Intraoperative measurement of LE compartment pressures for patients at especially high risk for compartment syndrome; 4. Interrupting prolonged lithotomy position by intermittently lowering the LEs to the level of the heart every 2 hours to ensure reperfusion of the LE; 5. Ensuring that the foot/ankle is not dorsiflexed, but rather, slightly plantar-flexed; and 6. Utilization of Allen™ stirrups instead of candy-cane stirrups [9,25,32,44]. Post-operative injury prevention measures include close monitoring with careful examination of the lower extremities immediately after surgery (with the patient awake so that disproportionate LE pain can be assessed for) with a high index of suspicion for compartment syndrome, which is critical to early diagnosis and mitigation of injury. It is our practice to document a physical exam of the LE in the operating room, immediately after removing the LE from the DL position, to confirm the absence of significant swelling or color change, and, upon awakening in the OR or recovery room, to assess that the patient can easily dorsi-flex and plantar-flex their feet, and to confirm the absence of disproportionate LE pain.
Table 3: Risk factors and preventative measures to reduce the risk of lower extremity injuries.
Our updated literature review confirms that the pathophysiologic mechanisms responsible for LE injuries during DL positioning are fairly well understood. A clinical review of our own gGAS patient series who underwent surgery in the DL position for an extended duration confirms that it is possible to avoid serious injuries when evidence-based precautions are integrated into operating room surgeons and nursing standard practices.
The emerging field of gender-affirming surgery permits patients the opportunity for growth in the care of this specific population. Given that these procedures are complex and require longer than average operative time, surgeons and operating room staff must make every effort to minimize the risk of lower extremity injuries during DL. Our described technique for protecting a patient’s lower extremities during DL focuses on specifically padding at-risk parts of the body, alerting co-surgeons, engaging staff and surgical assistants to never lean on any portion of the patient’s body, and, ‘proceduralize’ preventive care in collaboration with the operating room nursing staff, through scheduled “lower extremity checks”.
The proactive, interdisciplinary measures we describe for injury prevention are especially important as advanced age, body weight, incidence of concomitant chronic illness, and utilization of longer-duration surgeries, increase among our patient population.
Source of Funding: Dr. Richard Onofrio Cedars-Sinai Transgender Surgery and Health Program research fund Conflicts of Interest: S. Sandhu, S. Mallavarapu, and S. Smith: none; M. Garcia: MLM Sante, Inc. (CEO, Founder); and Safe Medical Designs, LLC (Co-founder, CMO); Ethicon (Paid educator); World Professional Association for Transgender Health (Paid educator).
- Association of Women’s Health, Obstetric and Neonatal Nurses. Lower Extremity Nerve Injury in Childbirth: AWHONN Practice Brief Number 11. J Obstet Gynecol Neonatal Nurs. 2020 Nov;49(6):622-624. doi: 10.1016/j.jogn.2020.08.004. Epub 2020 Oct 19. PMID: 33092945.
- Abdalmageed OS, Bedaiwy MA, Falcone T. Nerve Injuries in Gynecologic Laparoscopy. J Minim Invasive Gynecol. 2017 Jan 1;24(1):16-27. doi: 10.1016/j.jmig.2016.09.004. Epub 2016 Sep 14. PMID: 27639546.
- Akhavan A, Gainsburg DM, Stock JA. Complications associated with patient positioning in urologic surgery. Urology. 2010 Dec;76(6):1309-16. doi: 10.1016/j.urology.2010.02.060. Epub 2010 May 23. PMID: 20546878.
- Beraldo S, Dodds SR. Lower limb acute compartment syndrome after colorectal surgery in prolonged lithotomy position. Dis Colon Rectum. 2006 Nov;49(11):1772-80. doi: 10.1007/s10350-006-0712-1. PMID: 17036205.
- Sukhu T, Krupski TL. Patient positioning and prevention of injuries in patients undergoing laparoscopic and robot-assisted urologic procedures. Curr Urol Rep. 2014 Apr;15(4):398. doi: 10.1007/s11934-014-0398-1. PMID: 24574090.
- Ulm MA, Fleming ND, Rallapali V, Munsell MF, Ramirez PT, Westin SN, Nick AM, Schmeler KM, Soliman PT. Position-related injury is uncommon in robotic gynecologic surgery. Gynecol Oncol. 2014 Dec;135(3):534-8. doi: 10.1016/j.ygyno.2014.10.016. Epub 2014 Oct 23. PMID: 25449565; PMCID: PMC4268144.
- Vladinov GM, Glick B, Aguirre HO, Fiala RS, Maga JM. Lower Extremity Injury While Undergoing Urology Procedures in the Trendelenburg with Lithotomy Position: Three Case Reports. J Perianesth Nurs. 2021 Jun;36(3):214-218. doi: 10.1016/j.jopan.2020.08.010. Epub 2021 Apr 26. PMID: 33926806.
- Simms MS, Terry TR. Well leg compartment syndrome after pelvic and perineal surgery in the lithotomy position. Postgrad Med J. 2005 Aug;81(958):534-6. doi: 10.1136/pgmj.2004.030965. PMID: 16085748; PMCID: PMC1743337.
- Anderson MA, Burlingame B, Cahn JA, Conner R, Davidson D, deKay K, Fearon MC, Giarrizo-Wilson S, Johnstone EM, Jobman L, Jones E, Kelly J, Kyle E, Link T, Ogg MJ, Spruce L, Van Wicklin SA, Wood A, Wright R AORN Guidelines for Perioperative Practice - 2023 Ed.2023.
- Bouyer-Ferullo S. Preventing perioperative peripheral nerve injuries. AORN J. 2013 Jan;97(1):110-124.e9. doi: 10.1016/j.aorn.2012.10.013. PMID: 23265653.
- Cheney FW. The American Society of Anesthesiologists Closed Claims Project: what have we learned, how has it affected practice, and how will it affect practice in the future? Anesthesiology. 1999 Aug;91(2):552-6. doi: 10.1097/00000542-199908000-00030. PMID: 10443619.
- Agostini J, Goasguen N, Mosnier H. Patient positioning in laparoscopic surgery: tricks and tips. J Visc Surg. 2010 Aug;147(4):e227-32. doi: 10.1016/j.jviscsurg.2010.07.010. PMID: 20920906.
- Chaya BF, Berman ZP, Boczar D, Trilles J, Siringo NV, Diep GK, Rodriguez Colon R, Rodriguez ED. Gender Affirmation Surgery on the Rise: Analysis of Trends and Outcomes. LGBT Health. 2022 Nov;9(8):582-588. doi: 10.1089/lgbt.2021.0224. Epub 2022 Oct 14. PMID: 36251926.
- Fleisch MC, Bremerich D, Schulte-Mattler W, Tannen A, Teichmann AT, Bader W, Balzer K, Renner SP, Römer T, Roth S, Schütz F, Thill M, Tinneberg H, Zarras K. The Prevention of Positioning Injuries during Gynecologic Operations. Guideline of DGGG (S1-Level, AWMF Registry No. 015/077, February 2015). Geburtshilfe Frauenheilkd. 2015 Aug;75(8):792-807. doi: 10.1055/s-0035-1557776. PMID: 26365999; PMCID: PMC4554497.
- Donaldson J, Haddad B, Khan WS. The pathophysiology, diagnosis and current management of acute compartment syndrome. Open Orthop J. 2014 Jun 27;8:185-93. doi: 10.2174/1874325001408010185. PMID: 25067973; PMCID: PMC4110398.
- Torres PA, Helmstetter JA, Kaye AM, Kaye AD. Rhabdomyolysis: pathogenesis, diagnosis, and treatment. Ochsner J. 2015 Spring;15(1):58-69. PMID: 25829882; PMCID: PMC4365849.
- Wolthers SA, Lassen BV, Rasmussen LT, Rosenstock SJ, Foss NB. Position-Related Postoperative Peripheral Neuropathy After Laparoscopic Colorectal Surgery: A Comparative Single-Center Prospective Cohort Study. J Laparoendosc Adv Surg Tech A. 2022 Apr;32(4):349-354. doi: 10.1089/lap.2021.0021. Epub 2021 Jun 8. PMID: 34101493.
- Chen F, Wang X, Pan Y, Ni B, Wu J. The paradox of obesity in pressure ulcers of critically ill patients. Int Wound J. 2023 Sep;20(7):2753-2763. doi: 10.1111/iwj.14152. Epub 2023 Mar 17. PMID: 36932685; PMCID: PMC10410346.
- Prior DE, Ghosh PS. Postsurgical Inflammatory Sciatic Neuropathy. J Clin Neuromuscul Dis. 2021 Jun 1;22(4):237-238. doi: 10.1097/CND.0000000000000327. PMID: 34019013.
- Warner MA, Martin JT, Schroeder DR, Offord KP, Chute CG. Lower-extremity motor neuropathy associated with surgery performed on patients in a lithotomy position. Anesthesiology. 1994 Jul;81(1):6-12. doi: 10.1097/00000542-199407000-00004. PMID: 8042811.
- Bjøro B, Mykkeltveit I, Rustøen T, Candas Altinbas B, Røise O, Bentsen SB. Intraoperative peripheral nerve injury related to lithotomy positioning with steep Trendelenburg in patients undergoing robotic-assisted laparoscopic surgery - A systematic review. J Adv Nurs. 2020 Feb;76(2):490-503. doi: 10.1111/jan.14271. Epub 2019 Dec 2. PMID: 31736124.
- Koç G, Tazeh NN, Joudi FN, Winfield HN, Tracy CR, Brown JA. Lower extremity neuropathies after robot-assisted laparoscopic prostatectomy on a split-leg table. J Endourol. 2012 Aug;26(8):1026-9. doi: 10.1089/end.2011.0653. Epub 2012 Jun 13. PMID: 22515378.
- Rider Sleutel M, True B, Webb J, Valdez E, Van Thi Tran M. Integrative Review of Lower Extremity Nerve Injury During Vaginal Birth. J Obstet Gynecol Neonatal Nurs. 2020 Nov;49(6):507-524. doi: 10.1016/j.jogn.2020.09.155. Epub 2020 Oct 21. PMID: 33096043.
- Wassenaar EB, van den Brand JG, van der Werken C. Compartment syndrome of the lower leg after surgery in the modified lithotomy position: report of seven cases. Dis Colon Rectum. 2006 Sep;49(9):1449-53. doi: 10.1007/s10350-006-0688-x. PMID: 16937229.
- Mumtaz FH, Chew H, Gelister JS. Lower limb compartment syndrome associated with the lithotomy position: concepts and perspectives for the urologist. BJU Int. 2002 Nov;90(8):792-9. doi: 10.1046/j.1464-410x.2002.03016.x. PMID: 12406113.
- Maxon M, Cackovic C. Atraumatic Gluteal Compartment Syndrome Presenting in a Young Female with Unilateral Lower Extremity Symptoms. Case Rep Emerg Med. 2019 Jan 29;2019:7891275. doi: 10.1155/2019/7891275. PMID: 30838141; PMCID: PMC6374802.
- Dua RS, Bankes MJ, Dowd GS, Lewis AA. Compartment syndrome following pelvic surgery in the lithotomy position. Ann R Coll Surg Engl. 2002 May;84(3):170-1. PMID: 12092867; PMCID: PMC2503816.
- Goldsmith AL, McCallum MI. Compartment syndrome as a complication of the prolonged use of the Lloyd-Davies position. Anaesthesia. 1996 Nov;51(11):1048-52. doi: 10.1111/j.1365-2044.1996.tb15003.x. PMID: 8943599.
- Mabvuure NT, Malahias M, Hindocha S, Khan W, Juma A. Acute compartment syndrome of the limbs: current concepts and management. Open Orthop J. 2012;6:535-43. doi: 10.2174/1874325001206010535. Epub 2012 Nov 30. PMID: 23248724; PMCID: PMC3522209.
- Smith SM, Yuan N, Stelmar J, Pa-C GL, Gupta A, Kim HL, Garcia MM. An Alternative Option for Gender-Affirming Revision Vaginoplasty: The Tubularized Urachus-Peritoneal Hinge Flap. Sex Med. 2022 Dec;10(6):100572. doi: 10.1016/j.esxm.2022.100572. Epub 2022 Sep 29. PMID: 36183656; PMCID: PMC9780766.
- Garcia MM, Shen W, Zhu R, Stettler I, Zaliznyak M, Barnajian M, Cohen J, Sarin A, Nasseri Y. Use of right colon vaginoplasty in gender affirming surgery: proposed advantages, review of technique, and outcomes. Surg Endosc. 2021 Oct;35(10):5643-5654. doi: 10.1007/s00464-020-08078-2. Epub 2020 Oct 13. PMID: 33051762.
- Hara K, Kuroki T, Kaneko S, Taniguchi K, Fukuda M, Onita T, Sawai T. Prevention of well-leg compartment syndrome following lengthy medical operations in the lithotomy position. Surg Open Sci. 2020 Nov 11;3:16-21. doi: 10.1016/j.sopen.2020.10.001. PMID: 33305248; PMCID: PMC7709791.
- Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999-2010. JAMA. 2012 Feb 1;307(5):491-7. doi: 10.1001/jama.2012.39. Epub 2012 Jan 17. PMID: 22253363.
- Coleman E, Radix AE, Bouman WP, Brown GR, de Vries ALC, Deutsch MB, Ettner R, Fraser L, Goodman M, Green J, Hancock AB, Johnson TW, Karasic DH, Knudson GA, Leibowitz SF, et al. Standards of Care for the Health of Transgender and Gender Diverse People, Version 8. Int J Transgend Health. 2022 Sep 6;23(Suppl 1):S1-S259. doi: 10.1080/26895269.2022.2100644. PMID: 36238954; PMCID: PMC9553112.
- Eberhardt TD, de Lima SBS, de Avila Soares RS, Silveira LBTD, Rossarola Pozzebon B, Reis CR, Dos Santos KPP, Alves PJP. Prevention of pressure injury in the operating room: Heels operating room pressure injury trial. Int Wound J. 2021 Jun;18(3):359-366. doi: 10.1111/iwj.13538. Epub 2020 Dec 13. PMID: 33314605; PMCID: PMC8243998.
- Michaels MJ, Lish MC, Mohler JL. Patient positioning for radical retropubic prostatectomy. Urology. 1998 May;51(5):824-6. doi: 10.1016/s0090-4295(97)00687-0. PMID: 9610599.
- Practice Advisory for the Prevention of Perioperative Peripheral Neuropathies 2018: An Updated Report by the American Society of Anesthesiologists Task Force on Prevention of Perioperative Peripheral Neuropathies. Anesthesiology. 2018 Jan;128(1):11-26. doi: 10.1097/ALN.0000000000001937. PMID: 29116945.
- Association of Perioperative Registered Nurses. Recommended practices for positioning the patient in the perioperative practice setting. AORN J. 2001 Jan;73(1):231-5, 237-8. doi: 10.1016/s0001-2092(06)62092-9. Erratum in: AORN J 2001 Aug;74(2):201. PMID: 11201551.
- Dillavou ED, Anderson LR, Bernert RA, Mularski RA, Hunter GC, Fiser SM, Rappaport WD. Lower extremity iatrogenic nerve injury due to compression during intraabdominal surgery. Am J Surg. 1997 Jun;173(6):504-8. doi: 10.1016/s0002-9610(97)00015-9. PMID: 9207163.
- Johansson VR, von Vogelsang AC. Patient-reported extremity symptoms after robot-assisted laparoscopic cystectomy. J Clin Nurs. 2019 May;28(9-10):1708-1718. doi: 10.1111/jocn.14781. Epub 2019 Feb 1. PMID: 30653776.
- Canterbury TD, Wheeler WE, Scott-Conner CE. Effects of the lithotomy position on arterial blood flow in the lower extremities. W V Med J. 1992 Mar;88(3):100-1. PMID: 1574874.
- Chase J, Harford F, Pinzur MS, Zussman M. Intraoperative lower extremity compartment pressures in lithotomy-positioned patients. Dis Colon Rectum. 2000 May;43(5):678-80. doi: 10.1007/BF02235587. PMID: 10826430.
- Lachmann EA, Rook JL, Tunkel R, Nagler W. Complications associated with intermittent pneumatic compression. Arch Phys Med Rehabil. 1992 May;73(5):482-5. PMID: 1580778.
- Gupta A, Meriwether K, Tuller M, Sekula M, Gaskins J, Stewart JR, Hobson D, Cardenas-Trowers O, Francis S. Candy Cane Compared With Boot Stirrups in Vaginal Surgery: A Randomized Controlled Trial. Obstet Gynecol. 2020 Aug;136(2):333-341. doi: 10.1097/AOG.0000000000003954. PMID: 32649498.