More Information
Submitted: 11 June 2020 | Approved: 25 June 2020 | Published: 26 June 2020
How to cite this article: Wubneh M, Emishaw S. Animaw W. Level of Nurses to Patients Communication and Perceived Barriers in Government Hospitals of Bahir Dar City, Ethiopia, 2020. Clin J Nurs Care Pract. 2020; 4: 012-026.
DOI: 10.29328/journal.cjncp.1001023
Copyright License: © 2020 Wubneh M, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Communication; Barrier; Nurse-patient; Bahir Dar; Ethiopia; 2020
Level of Nurses to Patients Communication and Perceived Barriers in Government Hospitals of Bahir Dar City, Ethiopia, 2020
Moges Wubneh1*, Solomon Emishaw2 and Worku Animaw2
1Lecturer, Debre Tabor University, Ethiopia
2Assistant Professor, Bahir Dar University, Ethiopia
*Address for Correspondence: Moges Wubneh, Lecturer, Debre Tabor University, Ethiopia, Email: [email protected]
Background: Communication is the process of exchanging information or messages from one group to the other through mutually understood verbal or non-verbal ways. Communication barrier is anything that prevents receiving and understanding the messages. poor communication between patients and the nurses’ result in an increased length of stay, wastage of the resource, patient dissatisfaction, absence of confidence, and frustration for both the nurses and the patients. This study will provide basic information on the level of nurses to patients’ communication and perceived barriers in government hospitals of Bahir Dar city.
Objective: The objective of this study was to assess the level of the nurse to patient communication and perceived barriers in government hospital of Bahir Dar city, Ethiopia, 2020.
Methods: Institution based cross-sectional mixed-methods study was conducted from February 24 – March 9/2020 in government hospitals of Bahir Dar city. A total of 380 nurses were included in the quantitative study by using simple random sampling. For both the quantitative and qualitative study, at the initial stage of data collection and interview; informed consent was obtained from respondents. Data were entered into Epi Data 4.6 and analyzed with a statistical package of social science version 25. Data were mainly analyzed using descriptive statistics and binary logistic regression. For the qualitative study, purposive sampling technique was employed, and 7 participants were interviewed. Thematic analysis was used.
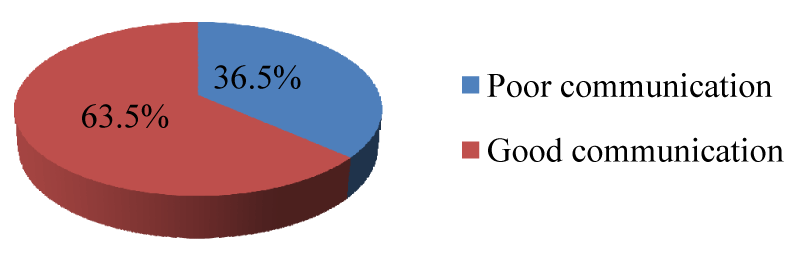
Results: From the total participants 36.5% of nurses were found to have poor communication. Variables which have statistically significant associations with the level of communication were educational level, work experience, the unwillingness of nurses, and lack of communication skill. The highest perceived communication barriers were lack of continuous training with 82.7% followed by workload with 80.7% and lack of medical facilities with 79.2% as reported by nurses. All environmental-related barriers were the perceived barriers of the nurse to patient communication.
Conclusion: In this study, the communication of nurses to patients is found to low. To enhance communication with the patients; nurses and other stakeholders like the ministry of health, the health bureau, and hospital authorities need to recognize the communication barriers. Giving awareness on the communication barrier for the nurses helps to minimize the barriers and improve the nurses to patients’ communication.
Background
Communication is the transfer of information by exchanging verbal and non-verbal messages. It is a core skill for all healthcare professionals and nursing staff in particular since nurses spend more time with patients and relatives than any other healthcare professional. When nurses communicate effectively with interest, listen actively, and demonstrate compassion, patients may be more likely to report their experiences as positive, even at times of distress and ill health [1].
Good communication between nurses and patients is essential for better care. They should also devote time to the patient to communicate with the necessary confidentiality, and must not forget that this communication includes persons who surround the sick person, which is why the language of communication should be understood by all those involved in it [2]. It can facilitate recovery, sense of safety and protection, improved patient satisfaction, and greater adherence to treatment options. Besides these, good communication through a patient-centered approach also serves to reassure relatives that their loved ones are receiving the necessary treatment [3]. Good communication has become increasingly reported as a key component in better nursing care outcomes [4]. Communication is a multi-dimensional, dynamic, and complex process that takes place in the hospital or related places. Nurses in hospitals need to enhance their skills in communication to improve patient satisfaction [5].
A communication barrier is anything that prevents from receiving and understanding the messages others use to share their information, ideas, and thoughts. Language barriers occur when people do not speak the same language, or do not have the same level of ability in a language. Such a language difference is causing an inability to exchange information and therefore a potential for misdiagnosis and mistreatment. Even with in the same language, there are vocabulary differences based on regions and professions. The nursing professions have their nomenclature that non-medical persons may not be able to understand. It also affected by time constraints, cultural differences, lack of knowledge and communication skills, nurse discomfort, and environmental factors which causes poor patient outcomes [4,6-9].
The studies in Manchester, England, and Canada indicated that poor communication between patients and the nurses’ result in an increased length of stay, wastage of the resource, patient dissatisfaction, absence of confidence and frustration for both the nurses and the patients [1,10]. Failure to recognize the two-way communication capability quite often leads to negative conclusions and attitudes. Moreover, the message sent is not the same as the message received. The decoding of the messages is based on individual factors and subjective perceptions. The receiver interprets the message they heard is not according to what the sender said but according to their code [2]. According to the research center for quality care, 10.8% of patients believed that nurses sometimes or never listened to them carefully, do not explain things clearly, and do not spend enough time with them [11].
In recent years the nurse to patient interaction is observed as an important element in nursing practice. Research findings from the United States, Australia, Norway, and Brazil have confirmed that there were problems on the patients’ side as a result of inadequate time given for them during nurse-patient engagement which in turn limits patients’ access to communicate their informational needs. Nurses do not understand communication as a key element to nursing care that should be used, especially at the time of the patient admission represented by feelings of fear, insecurity, and anxiety [8,12-14]. Evidence in Iran, Saudi Arabia, and Ghana showed that the patient, nurse, and environmental related issues affect the communication between nurses and patients which have the ultimate result in reducing good communication [4,9,15]. In Ethiopia, a study conducted in Jimma university hospital that assessed predictors of communication by patients’ point of view showed that therapeutic communication was poorly implemented [16]. But this does not show that the level of the nurse to patient communication and perceived barriers among nurses as the study participants. This is because the communication of patients can be determined by the communication capacity of nurses. So, if the nurses have good communication skills, the patients’ communication will be smoothed with their nurses. Even if, the Ethiopian ministry of health has implemented a compassionate respectful caring training program for health care workers including nurses to bring satisfaction to the patients; it might, unfortunately, helps to improve nurses’ communication with the patient. However the nurse to patient communication in the health institution not solved which observed as the obstacles of better care and patients suffered for long periods in the health institution without a listener and better care. Poor communication between nurses and patients increase mortality, morbidity, long hospital stay, increasing health care costs, and minimize clients’ attraction towards health institutions. Study findings will be used as input for decision-makers and responsible bodies like the federal ministry of health (FMOH), regional health bureaus, academic institutions, and health care professionals which helps to decide what needs to be done to improve nurses to patients’ communications. It will be used as baseline data for the researcher who needs to conduct on the area of the nurse to patient communication. Therefore the purpose of this study was to assess the’ level of the nurse to patient communication and perceived barriers in government hospitals of Bahir Dar city. In addition to these nurses’ experience on the nurse to patient communication barriers was explored.
Study setting
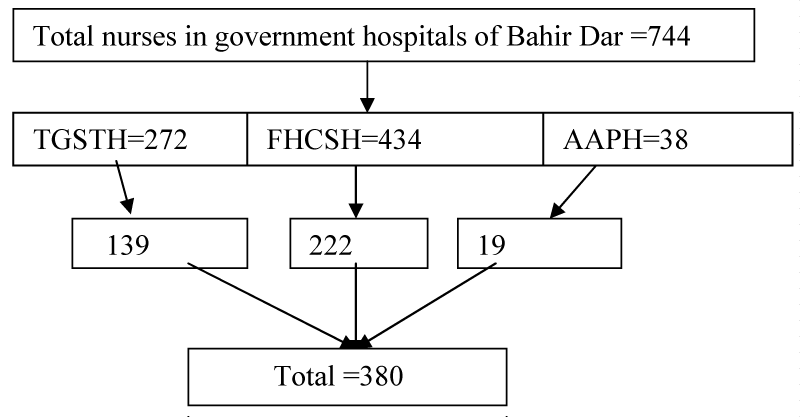
The study was conducted in Bahir dar city which is the capital city of the Amhara region located in 565 kilometers away from Addis Ababa in the NorthWest direction. There are three governmental hospitals in Bahir Dar city administration. These are Tibebe Gihon specialized- teaching hospital (TGSTH), Felege Hiwot comprehensive specialized hospitals (FHCSH), and Addis Alem primary hospital (AAPH). The total numbers of nurses in these three hospitals were 744 from February to March 2020.
Study design, population, sample size, and sampling procedure
An institutional-based cross-sectional mixed-method was used. The source populations were all nurses who work in government hospitals of Bahir Dar city, and nurses on sick leave or annual leave, and some other social problems were excluded. The total samples were 380 nurses for quantitative. First, the three governmental hospitals in Bahir Dar city were selected based on convenience because there are only three governmental hospitals, and private hospitals were not included because of the nurses in the governmental hospital also work at the private. Proportional allocation of samples based on the number of nurses was given for each hospital (Figure 1). Finally, nurses from each hospital were selected by simple random sampling using the lottery method. The sample size for qualitative was considered until data saturation, and 7 nurses were interviewed with data saturation was gained at the fourth participant. Data saturation is a matter of identifying redundancy in the data or relates to the degree to which new data repeat what was expressed in previous data during data collection [17]. The study was conducted from February – March 2020.
Figure 1: Schematic presentations of the sampling procedure.
Operational definition
Good communication: Those nurses’ who answered mean and above mean communication questions. That is there are 14 questions prepared to assess communication level with a Likert frequency scale (never, rarely, sometimes, often and always) with the value of 1 to 5. So the summation of the five Likert responses is 15 then divided by five which equals 3. Therefore the mean of one question is 3 and 42 is the mean of the 14 questions.
Poor communication: Those nurses who answered below mean communication questions.
Dependent variable
Level of the nurse to patient communication Independent Variables.
Age, sex, religion, marital status, educational level, position, work experience, working units, age difference, gender difference, language difference, religion difference, culture difference, Workload, shortage of nurses, low salary, lack of communication skill, unwillingness to communicate, nervous experience, dialect unfamiliarity, lack of time, problem out of work area, Family interference, pain, distrust of nurse competency, contagious disease, contact different nurses, presence of family on the bedside, Inappropriate room, busy environment, unfamiliar environment, lack of training, lack of facilities.
Data collection tool
A questionnaire assessing the level of nurses’ to patients’ communication and perceived barriers was adapted after a review of different works of literature [4,18,19]. The data collection instrument was prepared in English and translated to Amharic, and again re-translated to English by nurse academician. The pre-test was done in 5% of the calculated sample at Debre Tabor hospital to check whether the questions are simple, clear, and easily understandable. The questionnaire contained three sections. The first part included demographic part contains 8 questions, the second part was concerned with the perceived barriers of nurses to patients’ communication which contains 27 questions which were assessed by five-point Likert using agreement (strongly disagree=1, disagree=2, neutral=3, agree=4 and strongly agree=5) then which latter recorded or categorized as strongly disagree, and disagree=1, neutral=2, agree and strongly agree=3 for analysis; and the third part is about the level of communication which contains 14 questions with a minimum score of 14 and maximum of 70 scores. The validity of questionnaires’ was checked by expert opinion (face validity) [20]. Therefore the questionnaire’s validity was checked through face validity by four nurse academicians, one of them is an assistant professor, two lecturers, one assistant professor with a Ph.D. holder, and three clinical Bsc nurses who working at the hospitals. Internal consistency or reliability of the questionnaire was checked by using Cronbach’s alpha which was 0.919 for perceived barriers and 0.942 for the level of communication questions. An in-depth interview guide semi-structured questionnaire was used to elicit information concerned perceived communication barriers from the nurses’ point of view. Detailed information about nurses’ thoughts was explored in-depth which was offered a more complete picture of perceived barriers of the nurse to patient communication.
Data collection procedure
The data collection for a quantitative questionnaire was facilitated by BSc nurses, who had a better experience of data collection skills on clinical, and also training on data collection procedures and instruments were given. The data collectors distributed the self-administered questionnaire to the respondents to fill it. The qualitative data were collected by the principal investigator.
Data quality assurance
Adequate training and supervision were provided for the data collectors and supervisor. Codes were given to the questionnaires. The filled questionnaire was checked for completeness by data collectors and supervisors every day. Problems encountered during the study period were discussed in the study team and were solved. Computer frequencies and data sorting were used to check for missed variables, outliers, or other errors during data entry.
Data processing and analysis
Data were first checked for completeness and then each completed questionnaire assigned unique code. Subsequently, the data were entered using Epi Data 4.6. The generated data was exported to a statistical package for social sciences (SPSS) version 25. The data was cleaned by visualizing, calculating frequencies, and sorting. The analysis was done with descriptive statistics by using frequency, percentage, mean, median, and mode. Bivariate analysis between dependent and independent variables was performed using binary logistic regression by the enter method. Multicollinearity between independent variables was checked using the correlation coefficient. The correlation coefficients between predictor variables greater than 0.7 is an appropriate indicator for when collinearity begins to severely distort model estimation and subsequent prediction [21]. All explanatory variables which had an association in bivariate analysis with a p- value less than or equal to 0.25 were entered into a multivariable logistic regression model. Hosmer and Lemeshow test were checked for model goodness of fit (0.363). During the analyses, 0.05 P-value, and 95% confidence interval (CI) was used. A P-value of less than 0.05 was taken as a significant association. Results were presented in text, tables, charts, and graphs. Convergent parallel design (the quantitative and qualitative strands of the research are performed independently, and their results are brought together in the overall interpretation). In both quantitative and qualitative, the data collection and data analysis occur concurrently (QUAN + qual) and independently [22]. For the qualitative study field note and audio recorded was taken. Each interview was transcribed by cross-checked both the audio record and the field note. The accuracy of the transcripts was checked by repetitive listen to the audiotape and by reading the transcripts. The analysis was carried out by using deductive approach thematic analysis which involves coming to the data with some preconceived themes that expect to find reflected there, based on theory or existing knowledge [23]. Based on this data were thematized in four major themes. The themes included; common communication barriers with sub-themes of language difference; nurse related barriers with sub-themes of lack of communication skill, shortage of nurses and workload; patient-related barriers with sub-themes pain, and family interferences; environmental/health setting related barriers with sub-themes of lack of medical facilities and lack of continuous training, inappropriate and busy environment.
The integration was taking place in the results point of integration; in which writing down the results of the first component, the results of the second component are added and integrated [22]. The final result was triangulated to support the quantitative result.
Ethical clearance
Ethical issues within the study were taken into consideration when carried out the study. Ethical clearance was obtained from the institutional review board of Bahir Dar University, college of medicine, and health sciences with protocol number 0044/2020. A formal letter was submitted to Addis Alem primary hospital, Felege Hiwot hospital, and Tibebe Gihon hospital. For both the quantitative and qualitative study, at the initial stage of data collection and interview, informed consent was obtained from respondents and assured that their participation will be recorded anonymously, and confidentiality of response was maintained throughout the study.
Socio-demographic characteristics of the participants
A total of 380 samples were included in the study, and 370 participated with a response rate of 97.4%. The participants’ age ranged from 23 to 58 years, with a median age of 29 years. Among a total of participants, 189 (51.1%) were female (Table 1).
| Table 1: Socio-demographic characteristics of nurses in governmental hospitals of Bahir Dar city, Ethiopia, 2020(N=370). | |||
| Variables | Frequency(N) | Percent | |
| Age | 18-25 | 66 | 17.8 |
| 26-35 | 208 | 56.2 | |
| 36-45 | 76 | 20.5 | |
| 46 and above | 20 | 5.4 | |
| Marital status | Single | 181 | 48.9 |
| Married | 165 | 44.6 | |
| Separated | 24 | 6.5% | |
| Educational qualification | Diploma | 42 | 11.4% |
| Degree and above | 328 | 88.6% | |
| Experience | <2 years | 97 | 26.2% |
| 2-5 years | 85 | 23.0% | |
| 6-10years | 89 | 24.1% | |
| >10 years | 99 | 26.8% | |
| Working units | OPD | 98 | 26.5% |
| ICU | 67 | 18.1% | |
| Medical | 67 | 18.1% | |
| Surgery | 118 | 31.9% | |
| Obs/gyne | 20 | 5.4% | |
Level of communication
Nurse to patient communication is the exchange of information or message between nurses and patients.
About 135(36.5%) of the participants were found to have poor communication with 95%CI (31.9% - 41.9%) (Figure 1).
The communication level of nurses was assessed using 14 items of communication. The respondents’ score lies between a minimum of 14 to a maximum of 70. The mean used for dichotomous the data as poor and good communication was pre-determined (Table 2).
| Table 2: Communication items used to assess the level of the nurse to patient communication in governmental hospitals of Bahir Dar city, Ethiopia, 2020. | ||||||
| Items | Never | Rarely | Sometimes | Often | Always | Mea for each |
| You inform the patients right | 1 | 2 | 3 | 4 | 5 | 3 |
| You inform patients of the results when taking their vital signs (blood pressure, temperature, heart rate) |
1 | 2 | 3 | 4 | 5 | 3 |
| You give the patient information on any diagnostic tests(namely the type of test, its purpose, preparation and what will happen during the test) |
1 | 2 | 3 | 4 | 5 | 3 |
| You inform the patient about the medication-taking during hospitalization(kind, dose, side effects) |
1 | 2 | 3 | 4 | 5 | 3 |
| You keep patients informed on the condition of their health | 1 | 2 | 3 | 4 | 5 | 3 |
| You inform the family about the health conditions of critical patients and children |
1 | 2 | 3 | 4 | 5 | 3 |
| You try to include/inform them about the decisions related to their therapy |
1 | 2 | 3 | 4 | 5 | 3 |
| You provide information to the patients when they ask you | 1 | 2 | 3 | 4 | 5 | 3 |
| You are polite and friendly towards your patients(manner of speaking, protection of privacy, respect in diversity) |
1 | 2 | 3 | 4 | 5 | 3 |
| You immediately respond to their call for help(notification button, sign) |
1 | 2 | 3 | 4 | 5 | 3 |
| You inform the patients on how to take care of themselves at home after being released from the hospital |
1 | 2 | 3 | 4 | 5 | 3 |
| You inform the patients about positions which help to alleviate pain |
1 | 2 | 3 | 4 | 5 | 3 |
| You dedicate adequate time to communicate with patients | 1 | 2 | 3 | 4 | 5 | 3 |
| You respond to the patients’ concerns and complaints during their stay at the hospital |
1 | 2 | 3 | 4 | 5 | 3 |
| Overall mean score | 42 | |||||
Distribution of socio-demographic and perceived barrier variables and the level of communication
Those nurses qualified as degree and above 107 (79.2%) were had poor communication. Nurses less than 2 years of experience 48(35.5%) were had poor communication (Table 3a,b).
| Table 3a: Socio-demographics and perceived barrier variables and communication level of nurses in governmental hospitals of Bahir Dar city, Ethiopia, 2020 (N=370). | ||
| Variables | Level of communication | |
| Poor communication (N=135) | Good communication (N=235) | |
| Marital status | Single 80(59.3%) | 101(43%) |
| Married 50(37%) | 115 (48.9%) | |
| Separated 5(3.7) | 19(8.1%) | |
| Educational level | Diploma 28(20.8%) | 14(6%) |
| Degree and above107 (79.2%) | 221(94%) | |
| Experience | Less than 2 years 48(35.5%) | 49(20.9%) |
| 2-5 years 42(31.1%) | 43(18.3%) | |
| 6-10 years 29(21.5%) | 60(25.5%) | |
| Greater than10 years 16(11.9% | 83(35.3%) | |
| Work units | OPD 35(25.9%) | 63(26.8%) |
| ICU 23(17%) | 44(18.7%) | |
| Medical 24(17.8%) | 43(18.3%) | |
| Surgery 49(36.3%) | 69(29.4%) | |
| Obs/gyne 4(3%) | 16(6.8%) | |
| Religion difference | Disagree 72(53.3%) | 143(60.9%) |
| Neutral 8(6%) | 8(3.4%) | |
| Agree 55(40.7%) | 84(35.7%) | |
| Unwillingness of nurses | Disagree 32(23.7%) | 100(42.5%) |
| Neutral 12(8.9%) | 11(4.7%) | |
| Agree 91(67.4%) | 124(52.8%) | |
| Dialect unfamiliarity | Disagree 48(35.6%) | 116(49.3%) |
| Neutral 14(10.4%) | 23(9.8%) | |
| Agree 73(54% | 96(40.9%) | |
| Nervous experience | Disagree 52(38.5%) | 107(45.5%) |
| Neutral18 (13.3%) | 27(11.5%) | |
| Agree 65(48.2%) | 101(43%) | |
| Shortage of nurses | Disagree 25(18.5) | 45(19.1%) |
| Neutral 5(3.7%) | 19(8.1%) | |
| Agree 105(77.8%) | 171(72.8%) | |
| Lack of time | Disagree 17(12.6%) | 51(21.7%) |
| Neutral 6(4.4%) | 13(5.5%) | |
| Agree 112(83%) | 171(72.8%) | |
| Lack of communication skill | Disagree 28(20.7%) | 69(29.4%) |
| Neutral 4(3%) | 24(10.2%) | |
| Agree 103(76.3%) | 142(60.4%) | |
| New environments | Disagree 32(23.7%) | 73(31%) |
| Neutral 11(8.2%) | 22(9.4%) | |
| Agree 92(68.1%) | 140(59.6%) | |
| Contagious disease | Disagree 23(17%) | 59(25%) |
| Neutral 15(11.1%) | 21(9%) | |
| Agree 97(71.9%) | 155(66%) | |
| Distrust of competency | Disagree 27(20%) | 73(31.1%) |
| Neutral 8(5.9%) | 24(10.2%) | |
| Agree 100(74.1%) | 138(58.7%) | |
| Table 3b: Questionnaire used to assess the perceived barriers of the nurse to patient communication in governmental hospitals of Bahir Dar city, Ethiopia, 2020. | ||||||
| No | Questions | Answer | ||||
| 1 | Sex | 1. Male | 2. Female | |||
| 2 | Age | in year | ||||
| 3 | Marital status | 1 Single | 2.Married | 3.Widowed | 4.Divorced | |
| 4 | Religion | 1. Orthodox | 2. Muslim | 3. Protestant | 4. Catholic | 5. Other |
| 5 | Educational level | 1. Diploma | 2. BSc | 3. MSc | ||
| 6 | Position | 1.Nurse | 2.Head Nurse | |||
| 7 | Name of the section you are currently working on | |||||
| 8 | Service in year | No | Questions | Response | ||
| To what extent you agree that your communication with the patients will be affected as a result of; |
Strongly | Disagree | Neutral | Agree | Strongly Agree | |
| Common-related perceived barriers | ||||||
| 1 | Age difference between nurse and patient | 1 | 2 | 3 | 4 | 5 |
| 2 | Gender differences between nurse and patient | 1 | 2 | 3 | 4 | 5 |
| 3 | Cultural difference between nurse and patient | 1 | 2 | 3 | 4 | 5 |
| 4 | Religious difference between nurse and patient | 1 | 2 | 3 | 4 | 5 |
| 5 | Language differences between nurse and patient | 1 | 2 | 3 | 4 | 5 |
| Nurse - related perceived barriers | ||||||
| 6 | Unfamiliarity of nurses with dialect | 1 | 2 | 3 | 4 | 5 |
| 7 | Nurse's unwillingness to communicate with the patient | 1 | 2 | 3 | 4 | 5 |
| 8 | Nurse’s unpleasant experiences with patients | 1 | 2 | 3 | 4 | 5 |
| 9 | The place of nurses working | 1 | 2 | 3 | 4 | 5 |
| 10 | Having problems outside the working area | 1 | 2 | 3 | 4 | 5 |
| 11 | Shortage of nurses relatively to the patients' number | 1 | 2 | 3 | 4 | 5 |
| 12 | Work load of nurses | 1 | 2 | 3 | 4 | 5 |
| 13 | Not having enough time | 1 | 2 | 3 | 4 | 5 |
| 14 | Lack of communication skill | 1 | 2 | 3 | 4 | 5 |
| 15 | Low salary of nurses | 1 | 2 | 3 | 4 | 5 |
| Patient-related perceived barriers | ||||||
| 16 | patients resistance and unwillingness to communicate | 1 | 2 | 3 | 4 | 5 |
| 17 | the presence of pain | 1 | 2 | 3 | 4 | 5 |
| 18 | The presence of patients’ family or friend on the patient’s bedsides | 1 | 2 | 3 | 4 | 5 |
| 19 | The presence of family interference | 1 | 2 | 3 | 4 | 5 |
| 20 | Patient contact with different nurses | 1 | 2 | 3 | 4 | 5 |
| 21 | Distrust of patients by nurses competency | 1 | 2 | 3 | 4 | 5 |
| 22 | presence contagious disease | 1 | 2 | 3 | 4 | 5 |
| Environment-related perceived barriers | ||||||
| 23 | Patient presence in an unfamiliar environment | 1 | 2 | 3 | 4 | 5 |
| 24 | The busy environment (high noise and abundant traffic) | 1 | 2 | 3 | 4 | 5 |
| 25 | Inappropriate environmental conditions (inadequate ventilation in the environment, heat and cold, inappropriate light, Poor room sanitation, unpleasant odors, etc.) |
1 | 2 | 3 | 4 | 5 |
| 26 | Lack of continuing training in communication skills | 1 | 2 | 3 | 4 | 5 |
| 27 | Lack of facilities for patients | 1 | 2 | 3 | 4 | 5 |
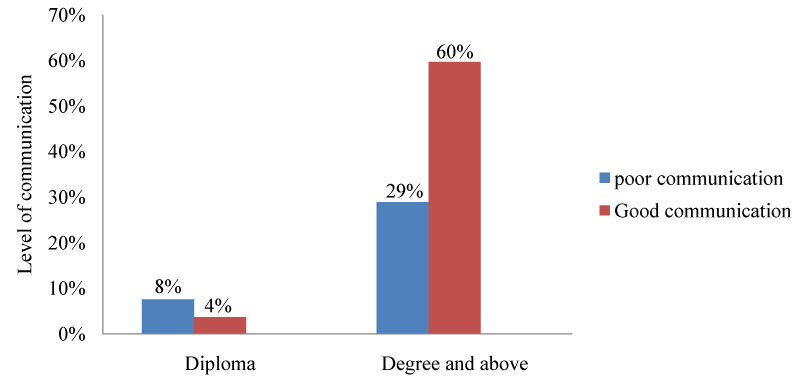
From the total respondents, diploma nurses 28 (8%), and qualified as a degree and above 107 (29%) were had poor communication (Figure 2).
Figure 2: The level of the nurse to patient communication in governmental hospitals of Bahir Dar city, Ethiopia, 2020.
Figure 3: Educational level of study participants and their level of communication in governmental hospitals of Bahir Dar city, Ethiopia, 2020.
Perceived nurse to patient communication barriers
Perceived communication barriers include socio-demographic characteristics nurses, common- related or perceived barriers on both sides, nurse-related, patient-related, and environment- related communication barriers.
Common-related perceived communication barriers reported by nurses
Barriers that are common between nurses and patients inhibited the communication of nurses with the patients.
Language difference was the highest perceived common-related communication barrier with a- mean score of 2.27, and 60.5% of nurses at 95% CI (49.7%, 70.4%) were agreed as a perceived common-related communication barrier with (median=3, mode=3), whereas religion difference was the least perceived barrier with a mean score of 1.795. But nurses disagreed with gender, culture, religion, and age differences (median=1, mode=1) (Table 4).
| Table 4: Perceived common communication barriers in governmental hospitals of Bahir Dar city, Ethiopia, 2020 (N=370). | ||||||
| Perceived barriers | Disagree | Neutral | Agree | Mean | Median | Mode |
| Language difference | 124(33.5%) | 22(6%) | 224(60.5%) | 2.27 | 3 | 3 |
| Gender difference | 208(56.2%) | 19(5.1%) | 143(38.6%) | 1.824 | 1 | 1 |
| Age difference | 207(55.9%) | 17(4.6%) | 146(39.5%) | 1.835 | 1 | 1 |
| Culture difference | 206(55.7%) | 27(7.3%) | 137(37%) | 1.814 | 1 | 1 |
| Religion difference | 215(58.1%) | 16(4.3%) | 139(37.6%) | 1.795 | 1 | 1 |
Nurses related communication barriers reported by nurses
Nurse related communication barriers are barriers to communication which make patients not having a good relationship with nurses.
The workload was the highest perceived nurse related communication barrier with a mean score of 2.66, and 80.8% participants at 95% CI (70.4%, 91.5%) were agreed as a barrier of communication, while unfamiliarity of the nurse with dialect was the least perceived communication barrier with a mean score of 2.01. About 74.6% of nurses also agreed that a shortage of nurses as a perceived communication barrier with 95% CI (65%, 83.9%). Workload, shortage of nurses, lack of time, lack of communication skills, problems outside the working area, nurses’ unwillingness to communicate, and low salary were the perceived communication barriers (median=3, mode=3). The nurses were tending to neutral or agree about the place of working, nurses’ unpleasant experiences, and unfamiliarity with dialect (median=2, mode=3) (Table 5).
| Table 5: Perceived nurse related communication barriers in governmental hospitals of Bahir Dar city, Ethiopia, 2020 (N=370). | ||||||
| Perceived barriers | Disagree | Neutral | Agree | Mean | Median | Mode |
| Work load | 54(14.6%) | 17(4.6%) | 299(80.8%) | 2.66 | 3 | 3 |
| Shortage of nurses | 70(18.9%) | 24(6.5%) | 276(74.6%) | 2.56 | 3 | 3 |
| Lack of time | 68(18.5%) | 19(5.1%) | 283(76.4%) | 2.58 | 3 | 3 |
| Low salary | 109(29.4%) | 34(9.2%) | 227(51.4%) | 2.32 | 3 | 3 |
| Lack of skill | 97(26.2%) | 28(7.6%) | 245(66.2%) | 2.4 | 3 | 3 |
| Problem out of working area | 120(32.5%) | 50(13.5%) | 200(54%) | 2.23 | 3 | 3 |
| Nurse's unwillingness | 132(35.7%) | 23(6.2%) | 215(58.1%) | 2.22 | 3 | 3 |
| work place | 154(41.6%) | 52(14.1%) | 164(44.3%) | 2.03 | 2 | 3 |
| unpleasant experiences | 159(43%) | 45(12.1%) | 166(44.9%) | 2.02 | 2 | 3 |
| Dialect difference | 164(44.3%) | 37(10%) | 169(45.7%) | 2.01 | 2 | 3 |
Patient-related barriers reported by nurses
There are patient-related issues that can inhibit nurse to patient communication; as a result, the care delivering to the patients and they expect to receive is not going harmoniously.
The presence of pain was the highest patient-related perceived communication barrier with the mean score of 2.5, and 70.8% of nurses were agreed as a barrier of communication with 95% CI (60.9%, 80.7%), whereas patients contact different nurses were the least perceived communication barrier reported by nurses with a mean score of 1.84. The nurses gave their agreement on pain, contagious disease, family interference, family or friends on the patient bedside, and distrust nurse competency (median=3, mode=3). Participants were tended to neutral about patients’ resistance or unwillingness to communicate (median=2, mode=3) and tended to neutral or disagree with patient contact different nurses (median=2, mode=1) (Table 6).
Table 6: perceived patient-related communication barriers in governmental hospitals of Bahir- Dar city, Ethiopia, 2020 (N=370). |
||||||
| Perceived barrier | Disagree | Neutral | Agree | Mean | Median | Mode |
| Pain | 81(21.9%) | 27(7.3) | 262(70.8%) | 2.5 | 3 | 3 |
| Distrust competency | 100(27%) | 32(8.6%) | 238(64.3%) | 2.37 | 3 | 3 |
| Contagious disease | 82(22.2%) | 36(9.7%) | 252(68.1%) | 2.46 | 3 | 3 |
| Family interference | 101(27.3%) | 24(6.5%) | 245(66.2%) | 2.389 | 3 | 3 |
| Family /friend on bedside | 98(26.5%) | 29(7.8%) | 243(65.6%) | 2.392 | 3 | 3 |
| Resistance /unwillingness | 154(41.6%) | 48(13%) | 168(45.4%) | 2.04 | 2 | 3 |
| Patient contact | 178(46.1%) | 74(20%) | 118(31.9%) | 1.84 | 2 | 1 |
Environmental related barriers reported by nurses
Nurse to patient communication is not only affected by patients and nurses alone but also the environment in which both interact together can decrease communication.
All environmental-related barriers were perceived as a communication barrier. Lack of continuous training on communication skills is the highest perceived communication barrier with the overall mean score of 2.71, and 82.7% of nurses at 95% CI (73.1%, 93.1%) were agreed as the barrier of communication, while the unfamiliar environment was the least perceived environmental or hospital-related communication barrier with the mean score of 2.34. Nurses were agreed that lack of medical facilities, busy environment, inappropriate environment, unfamiliar environment, and lack of training (median=3, mode=3) (Table 7).
| Table 7: perceived environment-related communication barriers in governmental hospitals of Bahir Dar city, Ethiopia, 2020 (N=370). | ||||||
| Perceived barriers | Disagree | Neutral | Agree | Mean | Median | Mode |
| Lack of training | 45(12.1%) | 19(5.1%) | 306(82.8%) | 2.71 | 3 | 3 |
| Lack of facilities | 60(16.3%) | 17(4.5%) | 293(79.2%) | 2.63 | 3 | 3 |
| Busy environment | 73(19.7%) | 23(6.2%) | 274(74.1) | 2.54 | 3 | 3 |
| Inappropriate environment | 73(19.7%) | 27(7.3%) | 270(73%) | 2.53 | 3 | 3 |
| Unfamiliar environment | 105(28.4%) | 33(8.9%) | 232(62.7%) | 2.34 | 3 | 3 |
Bivariate and multivariable logistic regression
From the total of eight socio-demographic and 27 perceived variables, 16 independent variables were associated with the outcome variables during bivariate analysis. Variables with a P value less than or equal to 0.25 were entered into multivariable logistic regression. But two variables which were age and culture difference (age with experience=0.747, culture with religion difference= 0.873) were dropped or not entered into multivariable regression because of multicollinearity. Finally, four variables were associated with the dependent variable. These were educational level, experience, the unwillingness of nurses for communication, and lack of communication skills. Those nurses who qualified degree and above were 6.14 times more likely with 95% CI 6.14(2.741, 13.764) to have good communication than diploma nurses. Those nurses who had work experience of 6-10 years were 3.5 times more likely with 95% CI (1.585, 7.748), and those who had greater than 10 years of experience were 12.85 times more likely with 95% CI (4.747, 34.762) to had good communication than those nurses who had less than two years of work experience. Nurses who agreed that unwillingness of nurses to communicate is a perceived communication barrier were 60.5% times less likely to have good communication than those who disagree (Table 8).
| Table 8: Bivariate and multivariable logistic regression in governmental hospitals of Bahir Dar city, Ethiopia, 2020. | |||||
| Variables | Category | COR (95% CI) | p - value | AOR (95% CI) | p -value |
| Marital status | Single | 1 | |||
| Married | 1.82(1.17 , 2.837) | 0.008 | 1.27(0.662, 2.422) | 0.475 | |
| Separated | 3(1.077 , 8.413) | 0.036 | 0.87(0.24, 3.182) | 0.837 | |
| Educational level | Diploma | 1 | |||
| Degree& above | 4.13(2.089 , 8.169) | 0.000 | 6.14(2.741, 13.764) | 0.000 | |
| Experience | <2 years | 1 | |||
| 2-5 years | 1.00 (0.56 , 1.8) | 0.992 | 1.60(.759, 3.294) | 0.221 | |
| 6-10 years | 2.03(1.1, 3.7) | 0.020 | 3.50(1.585, 7.748) | 0.002 | |
| >10 years | 5.08 (2.6, 9.9) | 0.000 | 12.85(4.747,34.762) | 0.000 | |
| Working section | OPD | 1 | |||
| ICU | 1.06(0.554 , 2.040) | 0.855 | 1.02(0.454, 2.279) | 0.967 | |
| Medical | 0.99(0.521, 1.903) | 0.989 | 0.90(0.406, 1.971) | 0.783 | |
| Surgery | 0.78(0.45, 1.359) | 0.383 | 0.61(0.3, 1,225) | 0.163 | |
| Obs/gyne | 2.2(0.689 , 7.167) | 0.181 | 3.10(0.799, 11.937) | 0.102 | |
| Religion | Disagree | 1 | |||
| difference | Neutral | 0.50(0.182, 1.396) | 0.187 | 0.83(0.228, 2.916) | 0.754 |
| Agree | 0.77(0.494,1.187) | 0.245 | 1.70(0.885, 3.273) | 0.111 | |
| Nurses | Disagree | 1 | |||
| unwillingness | Neutral | 0.293(0.118, 0.729) | 0.008 | 0.36(0.11, 1.212) | 0.100 |
| Agree | 0.436(0.269, 0.706) | 0.001 | 0.39(0.182, 0.856) | 0.019 | |
| Unfamiliar dialect | Disagree | 1 | |||
| Neutral | 0.68(0.323, 1.432) | 0.310 | 0.65(0.227, 1.850) | 0.417 | |
| Agree | 0.54(0.326, 0.857) | 0.009 | 0.55(0.266, 1.143) | 0.110 | |
| Nervous | Disagree | 1 | |||
| experience | Neutral | 0.73(0.368, 1.442) | 0.364 | 1.22(0.491, 3.007) | 0.679 |
| Agree | 0.76(0.479,1.190) | 0.226 | 1.60(0.779, 3.142) | 0.209 | |
| Shortage of nurses | Disagree | 1 | |||
| Neutral | 2.10(0.703, 6.341) | 0.183 | 2.6(.646, 10.245) | 0.180 | |
| Agree | 0.91(0.524, 1.562) | 0.719 | 2(.82, 4.704) | 0.130 | |
| Lack of time | Disagree | 1 | |||
| Neutral | 0.72(0.237, 2.196) | 0.566 | 0.64(0.143, 2.841) | 0.557 | |
| Agree | 0.51(0.280, 0.926) | 0.027 | 0.41(0.161, 1.028) | 0.057 | |
| Lack of skill | Disagree | 1 | |||
| Neutral | 2.44(0.774, 7.659) | 0.128 | 5.6(1.453, 21.601) | 0.012 | |
| Agree | 0.56(0.337, 0.929) | 0.025 | 0.88(0.397, 1.958) | 0.756 | |
| New environment | Disagree | 1 | |||
| Neutral | 0.88(0.381, 2.02) | 0.757 | 1.30(0.446,3.924) | 0.614 | |
| Agree | 0.67(0.408, 1091) | 0.107 | 1.10(0.516, 2.167) | 0.879 | |
| Contagious disease | Disagree | 1 | |||
| Neutral | 0.55(0.241, 1.238) | 0.147 | 0.64(0.224, 1.821) | 0.402 | |
| Agree | 0.62(0.361, 1.074) | 0.088 | 0.76(0.351, 1.637) | 0.480 | |
| Distrust | Disagree | 1 | |||
| competency | Neutral | 1.10(0.445, 2.767) | 0.824 | 1.30(0.394, 3.992) | 0.702 |
| Agree | 0.51(0.306, 0.851) | 0.010 | 0.81(0.375, 1.737) | 0.583 | |
Socio-demographic characteristics of nurses
A total of seven nurses have participated in the qualitative interviews, while 5(71.4%) of them were male. The age of the participants ranged from 38-50 with a mean age of 43.86 years.
Common communication barriers
Common barriers are those barriers that could arise from both sides of the nurse and patients which can decrease the nurses to patients’ communication. The barrier included under this was language difference.
Language differences
Persons without having common language cannot communicate effectively or properly to express their feeling as those who have a common language.
One of the participants said that the differences in language affect communication with the patients. The patients give other meanings as we told positive things for them. In this condition, I may no longer interest to communicate with such kind of patients (Participant 5).
The other nurse continued and he said we have face difficulty of communication with those patients who speak other than Amharic like “Awigna and Afan Oromo” language speakers cannot understand us whatever we talk good thing for them (Participant 6).
The 50 years old nurses spoken that language difference with the patients also affect our communication for example; we cannot easily communicate with those patients who speak “Agewigna” (Participant 1).
Nurse-related barriers
These are barriers that arise from the nurses, which can inhibit the nurse-patient communication. The barriers included under these were workload, shortage of nurses, and lack of communication skills.
Workload
The presence of workload from the nurses is the potential threat of better care. When nurses carry out activities more than their capacity they became burnout and unable to satisfy the patients’ care needs.
There is a shortage of nurses as a result we serve the patients more than our capacity and we feel fatigued, exhausted, and burnout. This damages our communication with the patients (Participant 3). The other participant also continued we face physical fatigue when we did more than our capacity; this leads to the obstacles of communication (Participant 6). I cannot give adequate time to communicate with the patients rather I prefer to do the routine activities because of workloads (Participant 7).
Shortage of nurses
The presence of inadequate nurses in the hospitals or few nurses during their shift can damage communication with their patients because of unable to address all demands of the patient very well.
“Especially at night shift nurse to patient ratio is one to ten up to twelve.” (Participant 5).
A 38 years old nurse said that there are a limited number of nurses compared to the flow of the patients. So during this time, we prefer to do our routine activities like medication administration, doing the nursing process without listening to the patient idea. As a result, our communication with patients is affected (Participant 4). The other nurse continued “we serve more than twenty patients especially during duty time” (Participant 6).
Lack of communication skill
Communication skill for nurses is very essential to communicate effectively with their patients. Nurses without good communication skill they cannot provide better care for the patients.
One nurse reported that “some nurses have natural behavior which may not shape with training” (Participant 2). The other nurse continued we most nurses have lacked the skill to communicate with the patient like the place we select for communication, how to start communication, and are patients understand me or not...is not considered (Participant 4). Some nurses cannot fully explain what things are going to do for their patients about care or treatments (Participant 6).
The other nurse said that I know one nurse she was assigned to work with me together in the pediatric ward. She was having an ethical problem. She made conflict most of the time with the patients. The entire mother knows her ethical problem and they always complained that we are not voluntary if our children’s medication is given by this red nurse. So this was the great barrier of communication with the patients (Participant 7).
Patient-related barriers
Patient-related barriers are these obstacles arise directly from the patients that inhibit nurse to patient communication. The barriers included under these were pain and family interference.
Presence of pain
Pain is a general term that describes uncomfortable sensations in the body. It can change the behavior of the patients from stable to irritable mood and results in refuses to make contact with their caregiver.
One nurse revealed that the presence of pain decreases the communication between nurses and patients. If the patients are in the good condition they have a good facial expression for nurses greeting but, if they are with the pain they cannot respond to our greeting (Participant 1).
The other participant also said that as the patients suffered by the pain, they are not voluntary to communicate with us (Participant 4). One of the participants also continued if the patients get pain they are not voluntary to communicate with the nurses (Participant 5). The 47 years old nurse said that patients with severe pain cause to disrupt our communication. Those patients are not voluntarily given accurate data to us unless we give anti-pain and got relive from pain (Participant 7).
Family interference
Conflict in the caring environment is common between care providers, and the patients’ attendants either intentionally or unintentionally. This is because of the unnecessary interferences of family or attendant with the caring process.
One of the nurses told that during we give care for the patients the family interferes with our activities. This makes angry for the nurses and leads to conflict with them and finally, communication with the patients inhibited. For example, one day the patient medication was discontinued in around session then the attendant comes and complained that why not you give the medication. The nurse responds for the attendant as it was discontinued, finally the attendant fight with the nurse why you discontinued it as it is already prescribed by the physician (Participant 5). The other nurse continued that at one time one college student come to us because of illness. During this time we were trying to help her but, her friends come and disturb us. They said this is not the disease rather she attacks by an evil eye person so, this cannot be treated by modern medicine, and they also try to hit one of the nurses with us (Participant 7).
Environmental-related barriers
These barriers are arising directly from the health care setting which caused the barrier of the nurse to patient communication. The barriers included under these were lack of continuous training, lack of medical facilities for the patients, Inappropriate and busy environment.
Lack of continuous training on communication
If nurses do not get continuous training regularly, they cannot update themselves and they may easily subject to tradition as well as lacked basic caring skills.
To increase our communication with the patients we need to have continuous training. But there is no training to enhance the nurse capacity especially on communication skills (Participant 4). The other nurse said that we need to have training on communications skill to enhance our communication with the patients (Participant 5). Lack of training on communication is the major barrier to communication with the patients. Short training needs to enhance the nurse to patient communication (Participant 7).
Lack of medical facilities
If the hospitals cannot provide the necessary medical equipment or materials for the patients; the patients complained goes to their immediate caregiver or nurses. This is the main cause of the communication barrier.
All participants said that a lack of medical facilities was a barrier to communication. One female nurse said the hospitals cannot provide all necessary medical facilities for the patients like a drug. For example, most societies in this surrounding area used health insurance. We prescribe drugs to the patients but they cannot get the drug inside the hospital rather they pushed to buy out of the hospital or in the private pharmacy. Then the patients complain to us as they cannot afford to buy the drug. We told the truth as it is not our responsibility and if hospitals can list out the non-available drug and post to the working unit we cannot prescribe it. They did not listen to us. This leads to conflict between nurses and patients and decreases communication (Participant 1). The other nurse continued that the health institution related issues are affecting our communication. For example, we send the patient to buy the drug out of the hospital then the patient made conflict with us. This is happening because the hospital cannot provide an adequate supply of drugs. This alters our communication with the patients (Participant 2).
The health insurance is another challenge for communication. The hospital cannot fulfill all the necessary drugs and the patients bought it out of the hospital. After that, they ask us to audit the cost of the drug. We respond to them our duties is to prescribe the drugs not auditing cost. This affects the communication we have with the patients (Participant 3). One male nurse also stated that “patient comes to the hospital with their health insurance, and drugs are not available adequately. During this time the patient is not interested to listen to us whatever we talk. This challenges our communication with the patients (Participant 4). The patients come with their health insurance, and they expect everything inside the hospital. If they did not get the services as they expected they shout towards us. In this condition, our communication with the patients is affected (Participant 5). Almost all persons use health insurance and the hospital cannot provide all the patient medical facilities like drug supply. If they cannot afford to buy the drug out of the hospitals their treatment may discontinue and they complain to us why the treatment discontinued. In this time we lead to an unnecessary verbal fight with the patients (Participant 6). Patients come with health insurance for free services but the hospital cannot provide all the services like drug supply; when they ordered to buy out of the hospital the make conflict with us (Participant 7).
Inappropriate environment
Unsafe caring environments are among the obstacles of the nurse to patient communication. Unattractive health care environments can hinder the interaction between nurses and patients.
Participants reported that poor sanitation of the room also affects the communication between nurses and patients (Participant 4&7).
Busy environment: Busy environment or the crowdedness of the health care environment is can inhibit nurse to patient communication.
One of the nurses said that the place of the hospital as it is nearing to the road the sound of the cars also affects us (Participant 5).
The other nurse also continued his idea for example when I enter the ward to care for my patient I saw the persons who make crowded rooms at that time I prefer to leave the room; because the environment was not suitable for me to communicate with my patient (Participant 7).
The main purpose of this study was to assess the level of the nurse to patient communication and perceived barriers in governmental hospitals of Bahir Dar city. Perceived communication barriers included common communication barriers; nurse-related, patient-related, and environmental-related barriers were assessed and explored in both quantitatively and qualitatively. The study participants were nurses working in governmental hospitals of Bahir - Dar city.
From the total of participants (N=370), 36.5% of nurses were had poor communication.
In this study, the proportion of poor communication is found to be high. This showed how much the communication level of nurses’ lies in difficult conditions and indicates that nurses did not get adequate communication skills in their training period at the college or university level. This result is higher than a study done in João Pessoa, Brazil showed that twenty-five percent of nurses inform their name and activity for the patient remained distant at the time of communication. This discrepancy is due to the nurses showed devote time to communicate with their patients compared to this study [14]. The finding is similar to the study done in Jimma, Ethiopia showed that nurses were had a low level of therapeutic communication [16].
Educational level, work experience, the unwillingness of nurses, and lack of communication skills were associated with the outcome variable. Language difference, workload, shortage of nurses, lack of time, lack of communication skills, problems outside the working area, nurses’ unwillingness to communicate, pain, distrust nurse competency, contagious disease, family interference, and family or friends on the patient bedside, lack of continuous training on communication skills, lack of medical facilities, busy environment, inappropriate environment, and unfamiliar environment were perceived communication barriers reported by nurses.
In this finding, diploma nurses are more likely to have poor communication than a degree and above-qualified nurses. This is obvious that being advanced from lower to higher-level education is expected to have better skill and knowledge because the required competencies seated in the curriculum bring this difference which is consistent with the evidence in British journal of nursing supports that degree nurses were showed genuine differences in clinical practice than diploma nurses [24]. In this study nurse who had less than two years of work experience were more likely to have poor communication than those who had work experience of 6-10 and greater than10 years of work experience; which is consistent with the study done in China, found that as the nurses became experienced their communication level gets improved. Those who experienced two to three years were lacked communication skills with their patients [25]. Evidence in Saudi Arabia also showed that nurses with shorter experience perceived more barriers to communication than nurses with longer experience [4]. This is because while nurses get more experienced, they might be acquired different communication skills or techniques that how they can approach and communicate with their patients than the less experienced or newly employed nurses.
Language difference was perceived common-related communication barrier reported by nurses. As the qualitative finding also supported that language difference affect nurse to patient communication. This because of the presence of multilingual people in Ethiopia including the study area can be the barrier of communication. This result is consistent with the studies done in Saudi Arabia in which nurses were reported that they faced difficulty in dealing with patients because of language differences [26]. Another study in Saudi Arabia also supported this finding in which some of the communication practices rely on non-verbal methods due to a lack of a common language which often results in misinterpreted in the meaning of the communication [27].
In this study, nurses agreed that workload was the barrier of the nurse to patient communication which is also supported in the qualitative result of this study. Because when nurses working beyond their capacity they become exhausted and burnout as a result they cannot easily interact or communicate with their patients. This result is in line with a study conducted in Ghana; in which nurses were agreed that overwork as the barrier of communication [15]. This finding also supported by the studies done in two different areas of Iran indicated that workload was the barrier of communication between nurses and patients [28,29]. It also supported by a study in Saudi Arabia in which nurses were agreed that heavy workload as a barrier of the nurse to patient communication [4].
Nurses agreed that the shortage of nurses was barrier communication as participants in qualitative interviewees also strengthen this idea. The main reason is in this area the nurse to patient ratio reaches to one to twenty or more compared to in the state of California the maximum nurse to patient ratio is one to six [30]. This finding is similar to a study done in Ghana in which nurses agreed that shortage of nurses as barrier communication [15]. Other Studies in two different areas of Nigeria also supports that inadequate or shortage of nurses was affect the nurse to patient communication [31,32].
Lack of time also another communication barrier reported by nurses. This is because, if the nurses carry a high burden of activities, they do not have adequate time to communicate with the patients. This result is aligned with the study done Egypt, and in two different areas of Nigeria, and Ghana showed that lack of time was the barrier communication between nurses and patients [15,31-33].
Nurses agreed that Problems outside the working area were a barrier of communication, but a study done in Saudi Arabia showed that there was disagreement about problems outside work as a barrier to communication [4]. The difference is due to the work experience of nurses in Saudi - Arabia was from 1-24 months and since most of the nurses were freshmen for the working area, they might not be encountered problems out of working area compared to these study participants.
Nurses’ unwillingness to communicate found to be the barrier of the nurse to patient communication. This is due to the presence of a lack of communication skills in the nurses. This is supported by studies done in Singapore and Ghana showed that nurses were more reluctant or lack of interest to engaged in communication which caused communication barrier between nurses and patient [18,34].
In this study low salary paid for nurses was the barrier of communication. The reason is that if the nurses cannot be paid based on the task performing, they will not get satisfied with their work and result in a decrease in engaging in communication with patients. This is aligned with a study done in Saudi Arabia nurses were agreed that low salary was one of the perceived communication barriers [4].
More than seventy percent of nurses agreed that the presence of pain was a barrier of communication which also supported by the qualitative results. The main reason that patients seek to visit health institutions is because of pain. If pain cannot manage properly, the patients do not have the interest to communicate with their caregiver. This study is consistent with a study done in Ghana indicated that Pain was the major patient-related barriers to communication which accounts for eighty percent of respondents [15].
The finding indicates that the presence of contagious disease was one of the perceived communication barriers. This is because nurses afraid acquiring of communicable or contagious disease from the patients, they prefer to away from the patient and lead to a decrease in the nurses’ interaction with their patients. This result is similar to the studies done in Iran that showed that the obstacle of communication was the influence of contagious diseases [28,35]. It also supported by a study done in Saudi Arabia [4].
In this study family interference is the other barrier of the nurse to patient communication both in quantitative and qualitative results. It is due to the interference of family members in the patient caring process unnecessarily, the nurse preferred to leave the patient. This is aligned with the study done in Saudi Arabia, and a qualitative study in Ghana indicated that family interference was the barrier of Communication [4,18].
Nurses agreed that distrust nurse competency is the main communication barrier. This is happening because patients and their attendants do not give enough credit for the work of nurses. This finding is supported by a study done in Singapore which showed that nursing has a low occupational prestige; as a result, communication was greatly inhibited as patients see nurses similar to foreign domestic workers [34].
In this study, nurses agreed that the lack of continuous training on communication skills was the major barrier of communication, and participants’ in-depth interviewees also supported this finding. This because nurses without adequate continuous training on communication skills can easily vulnerable to poor communication. This result is similar to the study done in Saudi Arabia indicated that there was general agreement among the nurses that lack of continued training in communication skills was seen as a communication barrier between nurses and patients [4].
Both quantitative and qualitative finding shows lack of medical facilities is the barrier of the nurse to patient communication. Because patients come to the hospitals to get adequate services, if not this, patients make conflict with the frontline caregiver or nurses. This result is similar to the study done in Egypt showed that there were inadequate facilities that affect patients’ communication with nurses [33]. It also supported by the study done in Saudi Arabia nurses were showed their agreement as a barrier of communication [4].
In this study, both quantitative and qualitative findings show that a busy environment is one of the environmental-related communication barriers. Unsafe environments make boredom relationships between nurses and patients as a result they cannot create comfortable conversations on both sides. It aligned with studies done in Isfahan Iran, Ghana, and Egypt showed that busy or crowded rooms were the main environment-related communication barrier [15,33,35].
In this study unfamiliar environment was the barrier of communication as reported by nurses. When the patients are new to the health institution or hospitals, they faced different challenges like anxious interaction with caregivers and unable to find different service rooms in the hospital. This result is similar to the studies done in two different areas of Ghana indicated that nurse to patient communication was affected when patients new to the hospitals [15,18].
Generally, the finding revealed that nurses have found to be at a poor level of communication. There are perceived communication barriers including socio-demographics, common related, nurse related, patient-related, and environmental or hospital-related barriers which affect nurse to patient communication. There was the correspondence of results in both quantitative and qualitative methods or the findings in qualitative in-depth interviewees used to support the quantitative results. The result of this study has multidimensional implications. It can be used for the nurses to deal with and overcome the communication barriers. Dealing with the communication barriers mean also dealing with the problems of the patients so that the patients can get better care from their caregiver. As the barrier going to be minimizing or decreasing, the hospitals can be attractive for patients, safe for healing, increasing patient satisfaction, decrease hospital stay, and helps to minimize health care costs. Finally, this finding can be used as a baseline for further research.
Strength of the study
The study employed a mixed-methods design which helps to triangulate the quantitative findings by the qualitative findings.
Limitations of the study
This study was focused on nurses’ perception only; perceptions of patients on the communication barrier were not assessed and explored. As the response of the questionnaires was prepared by a Likert scale; there might be social desirability bias.
In this study, the communication of nurses to patients is found to low. Nurse to patient communication can be achieved by investing in continuous education as a way to enlighten professionals on the purpose of communication. Nurses, patients, and the environments are the main perceived communication barriers as indicated in both quantitative and qualitative methods. Lack of medical facilities or access is the main barrier of the nurse to patient communication which needs great attention of the stakeholders. Nurse professionals need to have good communication skills to solve or overcome the problem of patients; and must communicate effectively to perform their roles as educators, managers, decision-makers, client advocators, problem solvers, and caregivers. To enhance communication with the patients; nurses and other stakeholders like the Ministry of health, health bureau, and hospital authorities need to recognize the communication barriers. Giving awareness on the communication barriers for the nurses helps to minimize the barriers and improve the nurses to patients’ communication.
I would like to thank Bahir Dar University; for giving me this chance to attend a master’s program in adult health nursing; and Debre Tabor University for sponsoring me to do this research. Then, I would like to give my deepest gratitude to my advisors Mr. Solomon Emishaw and Dr. Worku Animaw (PhD.) for their unreserved advising to accomplish this thesis. I would like to extend my thanks also to my friends Mr. Tigabu Dessie and Mr. Nigus Solomon for their advice. Finally, I would like to thank the clinical nursing directors of the three governmental hospitals in Bahir Dar city, for all their necessary collaboration; data collectors, and all study participants who actively involved directly or indirectly for the accomplishment of this thesis.
- Elaine B. Effective communication skills in nursing practice. Nurs Stand. 2014; 29: 53-59. PubMed: https://pubmed.ncbi.nlm.nih.gov/25467362/
- Lambrini K, Papathanasiou Ioanna V. Communication in nursing practice. Mater Sociomed. 2014; 26: 65-67. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3990376/
- Ros W. Effective communication skills for the “caring” nurse. The Great Teachers: Tertiary Place. 2012.
- Albagawi Bander S, Jones Linda K. Quantitative exploration of the barriers and facilitators to nurse-patient communication in Saudi Arabia. J Hospital Admin. 2017; 6: 16.
- Andriyanto. Communication barrier between nurse and patient at the hospital: A systematic review. J Health Policy Management. 2019; 4: 105-110.
- Usha RK. Communication barriers. 2016.
- Bridges J, Nicholson C, Maben J, Pope C, Flatley M, et al. Capacity for care: Meta‐ethnography of acute care nurses' experiences of the nurse‐patient relationship. J Adv Nurs. 2013; 69: 760-772. PubMed: https://pubmed.ncbi.nlm.nih.gov/23163719/
- Bronwyn H, Susan B, Linda W. Nursing the patient with complex communication needs: Time as a barrier and a facilitator to successful communication in hospital. J Adv Nurs. 2012; 68: 116-126. PubMed: https://pubmed.ncbi.nlm.nih.gov/21831131/
- Roohangiz N, Maryam A, Maryam S, Mehrdad K, Elham S. Communication barriers perceived by nurses and patients. Glob J Health Sci. 2015; 8: 65-74. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4954910/
- Steve H, Elena H. Barriers to the practice of rural and remote nursing in Canada. European Sci J. 2016; 12: 7857-7881.
- Zamanzadeh V, Rassouli M, Abbaszadeh A, Nikanfar A, Alavi-Majd H, et al. Factors influencing communication between the patients with cancer and their nurses in oncology wards. Indian J Palliative Care. 2014; 20: 12-20. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3931236/
- Gørill H. Nurse–patient interaction is a resource for hope, meaning in life, and self‐transcendence in nursing home patients. Scand J Caring Sci. 2014; 28: 74-88. PubMed: https://pubmed.ncbi.nlm.nih.gov/23461626
- Sue L. “The button” initiating the patient-nurse interaction. Clin Nurs Res. 2014; 23: 188-200. PubMed: https://pubmed.ncbi.nlm.nih.gov/23524539
- Rezende LCM, De Freitas Macedo Costa KN, Martins KP, Da Costa TF, Dos Santos SR, et al. Therapeutic communication between nurses and patients in pre-operative during an admission in a medical surgical unit. Surgery. 4:5.
- Amoah VMK, Anokye R, Boakye DS, Acheampong E, Budu-Ainooson A, et al. A qualitative assessment of perceived barriers to effective therapeutic communication among nurses and patients. BMC Nursing. 2019; 18: 4. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/30792611
- Olana FR, Masresha A, Asresash D, Tefera B. Predictors of therapeutic communication between nurses and hospitalized patients. Heliyon. 2019; 5: e02665. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6838810/
- Benjamin S, Sim J, Kingstone T, Baker S, Waterfield J, et al. Saturation in qualitative research: Exploring its conceptualization and operationalization. Quality & quantity. 2018; 52: 1893-1907. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/29937585
- Amoah VMK, Reindolf A, Serwaa BD, Naomi G. Perceived barriers to effective therapeutic communication among nurses and patients at Kumasi south hospital. Cogent Medicine. 2018; 5: 1459341.
- Peleki T, Resmpitha Z, Mavraki A, Linardakis M, Rikos N, et al. Assessment of patients' and nurses' opinions on bidirectional communication during hospitalization: A descriptive study. Health Sci J. 2015; 9: 1.
- Bolarinwa OA. Principles and methods of validity and reliability testing of questionnaires used in social and health science researches. Nigerian Postgraduate Medical Journal. 2015; 22: 195-201. PubMed: https://pubmed.ncbi.nlm.nih.gov/26776330/
- Dormann Carsten F, Elith J, Bacher S, Buchmann C, Carl G, et al. Collinearity: A review of methods to deal with it and a simulation study evaluating their performance. Ecography. 2013; 36: 27-46.
- Schoonenboom J, Johnson RB. How to construct a mixed methods research design. Kolner Z Soz Sozpsychol. 2017; 69: 107-131. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5602001/
- Victoria C, Braun V, Hayfield N. Thematic analysis. Qualitative psychology: A Practical Guide Res Methods. 2015: 222-248.
- Swindells C, Willmott S. Degree vs diploma education: Increased value to practice. Br J Nurs. 2003; 12: 1096-1104. PubMed: https://pubmed.ncbi.nlm.nih.gov/14581843
- Angela CE, Lik TP, Yin CSS, Wong FY, Winsome L. Nurses’ perspectives on their communication with patients in busy oncology wards: A qualitative study. PloS One. 2019; 14. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6812861/
- Al-Harasis S. Impact of the language barrier on quality of nursing care at armed forces hospitals, Taif, Saudi Arabia. Middle East J Nurs. 2013; 101: 1-8.
- Mukhlid A, Jed D, Michelle G. Barriers to nurse-patient communication in Saudi Arabia: An integrative review. BMC Nurs. 2019; 18: 61.
- Anoosheh M, Zarkhah S, Faghihzadeh S, Vaismoradi M. Nurse–patient communication barriers in Iranian nursing. Int Nurs Rev. 2009; 56: 243-249. PubMed: https://pubmed.ncbi.nlm.nih.gov/19646175
- Kargar JM, Somayeh R. Evaluation of barriers contributing to the demonstration of effective nurse-patient communication in educational hospitals of Jahrom, 2014. Global J Health Sci. 2014; 6: 54-60. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/25363103
- Lippincott. The importance of the optimal nurse-to-patient ratio Nov 10 2016.
- Taiwo AO. Effect of communication on nurse-patient relationship in national orthopedic hospital, Igbbobi, Lagos. West African J Nurs. 2014; 25.
- Christianah OO, Oluwakorede O. Peplau’s theory of psychodynamic nursing and nurse-patient interaction: A literature review.
- Fathi IA, Mohammed TF, Akel Dalal T. Nurse communication in health education: Patients’ perspective. Clinical Nursing Studies. 2015; 3: 94-102.
- Hui TL, Desley H, Emily A. Factors affecting effective communication between registered nurses and adult cancer patients in an inpatient setting: A systematic review. Int J Evid Based Healthcare. 2011; 9: 151-164. PubMed: https://pubmed.ncbi.nlm.nih.gov/21599844/
- Soheyla B, Shahla M, Zahra M. Obstacles in nurse - elderly relationship from the patients' points of view. 2009.