More Information
Submitted: 07 November 2019 | Approved: 04 December 2019 | Published: 05 December 2019
How to cite this article: Gezie H, Leta E, Admasu F, Gedamu S, Dires A, et al. Health care workers knowledge, attitude and practice towards hospital acquired infection prevention at Dessie referral hospital, Northeast Ethiopia. Clin J Nurs Care Pract. 2019; 3: 059-063.
DOI: 10.29328/journal.cjncp.1001019
ORCiD: orcid.org/0000-0001-6486-9125
Copyright License: © 2019 Gezie H, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Health care workers; Hospital acquired infection; Infection prevention; Knowledge; Attitude; Practice; Dessie referral hospital
Abbreviations: CNS: Central Nervous System; DRH: Dessie Referral Hospital; HAI: Hospital Acquired Infection; HAIPs: Hospital Acquired Infection Preventions; HCWs: Health Care Workers; IESO: Integrated Emergency Surgery Officer; KAP: Knowledge, Attitude and Practice; PPE: Personal Protective Equipment; SPSS: Statistical Package for Social Sciences; TB: Tuberculosis; UTI: Urinary Tract Infection; VAP: Ventilator Associated Pneumonia
Health care workers knowledge, attitude and practice towards hospital acquired infection prevention at Dessie referral hospital, Northeast Ethiopia
Hailemariam Gezie1, Emebet Leta2, Fikrte Admasu2, Sisay Gedamu1*, Abebe Dires1 and Debrnesh Goshiye1
1School of Nursing and Midwifery, College of Medicine and Health Sciences, Wollo University, Ethiopia
2Debrebirhan, North Shewa Zone, Amhara Regional State, Ethiopia
*Address for Correspondence: Sisay Gedamu, Lecturer in School of Nursing and Midwifery, College of Medicine and Health Sciences, Wollo University, Ethiopia, Tel: +251920553732; +251935574801; Email: [email protected]
Introduction: Contact of health care workers and patient at health facility lead to the transmission of pathogenic organisms to each other. Hospital acquired infection prevention is standardized guide lines contain multitude protocols needed to be implemented by health care workers to reduce hospital acquired infections.
Objective: To assess health care workers knowledge, attitude and practice towards hospital acquired infection prevention at Dessie referral hospital.
Method: Institutional based cross sectional study was conducted among health care workers. The subjects were selected by proportional allocation in each respective department and simple random sampling method was employed. Statistical package for social sciences (SPSS) was used to analyze the data and presented in frequency tables and graph.
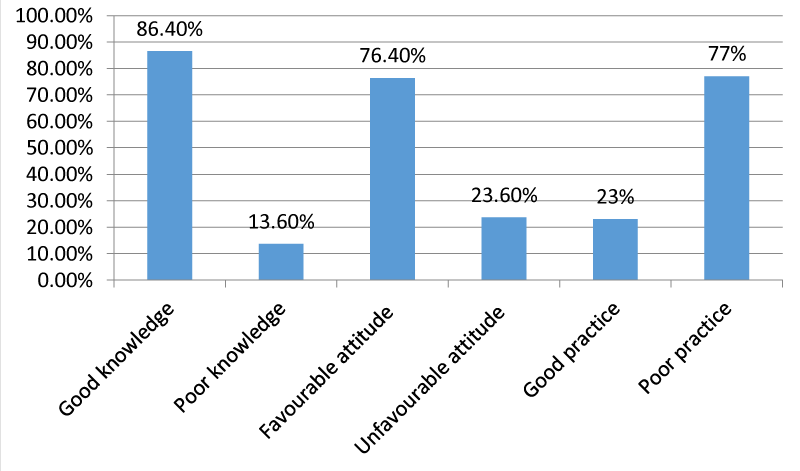
Results: 191 study subjects were participated in the study which gives a response rate of 90.5% from 211 total sample sizes. The study subjects had given their response according to self-administered questioner. The result indicates that 86.4%, 76.4% and 77% of respondents had good knowledge and favorable attitude and poor practice towards hospital acquired infection prevention respectively.
Conclusion: Even though the majority of the health care workers had good knowledge and favorable attitude, more than two third of them had poor practice towards hospital acquired infection prevention. Therefore health workers should strictly follow hospital acquired infection prevention guidelines. Improving sustainable supplies like personal protective equipment, water supply and hand washing facilities at patient care site is vital to correct the poor practice of infection prevention.
Hospital acquired infections or nosocomial infections are common worldwide problems mainly in developing and middle- income countries but it also affects developed countries [1]. The most common health care associated infections include; pneumonia (21.8%), surgical site infection (21.8%), gastrointestinal infections (17.1%), urinary tract infection (UTI) (12.9%) primary blood stream infections (9.9%), eye, ear, nose, throat, mouth infections (5.6%), lower respiratory tract infections (4.0%), skin and soft tissue infections (3.2%), cardiovascular infections (1.2%), bone and joint infections (1.0%), Central nervous system (CNS) infections (0.8%), reproductive tract infection (0.6%), and systemic infections (0.2%). These infections are mostly caused by bacteria such as E. coli, Staphylococcus aurous, Streptococcus and clostridium species, and other non-bacterial microorganisms like fungus, viruses and other parasites [2]. These infections usually acquired during patient examination, operation, specimen collections, handling of instrument, discarding of left over specimens and used equipment [3-5].
Hospital acquired infection (HAI) continues to be burden to the world health care system through increased risk to patient and employees. These infections have remarkable health and financial costs with an estimate incidence of 2,000,000 infection per year, 20,000 death per year and increased costs of billion dollars per year [6]. It is also estimated that more than 1.4 million people worldwide suffering from HAI. Approximately in the United States, 2 million patients develop HAI, and nearly 90,000 of these patients are estimated to die. In Sub-Saharan countries the problems associated HAIs hampered by inadequate data. However, prevalence from some African countries reported that high infection rates (Mali 18.9%, Tanzania 14.8%), rates of infection can exceed 20% [7]. Study in Ethiopia revealed that high prevalence of both life times (28.8%) and one year (20.2%) HAI exposure among health care workers (HCWs) [8].
Hospital acquired infection prevention (HAIP) is standardized guide line contain multitude protocols needed to be implemented by HCWs to reduce HAIs [9]. But several factors such as poor awareness among HCWs, compliance associated with personal, logistical and organizational barriers have negative effect on proper application of HAIP protocols [10].
Figure 1: Overall health care workers knowledge, attitude and practice towards hospital acquired infection prevention at DRH, Ethiopia.
HAIP which is the back bone of reducing HAIs didn’t get enough attention in Ethiopia. Moreover, in our study area there is scarcity of studies on health care workers knowledge, attitude and practice (KAP) towards HAIPs so that we tried to investigate KAP of Dessie referral hospital (DRH) health workers towards HAIP in order to indicate measures to be taken to address the problem.
Study design, setting and period
Facility based cross sectional study was conducted in Dessie referral hospital among health care workers to assess their KAP towards HAIP from March 11-17, 2017. DRH found in Dessie town, Amhara region, North east Ethiopia, 401 km away from Addis Ababa, the capital of Ethiopia and 480 km from Bahirdar, capital of Amhara regional state. This hospital gives many services including preventive, curative and rehabilitative care for patients coming from all woredas and zones of Eastern Amhara and Afar regional state.
Population
This study was done on HCW working in DRH. Those HCW providing health care service during data collection period were included in the study. HCW who were not providing service during the study period such as health workers who were on annual breaks and educational leave were excluded in this study.
Sample size determination and sampling technique
The sample size was determined by using single population proportion formula, the level of confidence = 95% (Z = 1.96), degree of precision (marginal error) = 5% and by taking estimate of prevalence towards HAIP practice = 54.2% [11]. Based on this assumption, the sample size for the study was 381. Since total population is 388 which is less than 10,000; we used population correction formula, we got 192. Then by adding 10% for non-response rate the final sample size was 211 health care providers. To select the study participants, the total sample size was allocated proportionally based on the number of professional size in each department. Finally, from each department, health workers were selected by using simple random sampling method to attain the final individuals.
Data collection tools and procedure
Self-administered questionnaire was used for data collection. It includes four parts; the first section containing socio demographic characteristics such as age, sex, educational status, work experience and profession. The second part elicits about knowledge, the third part includes questions concerning attitude and the last part includes practice assessment questions towards infection prevention. Before data collection one day training was given for data collectors and supervisor regarding the study, the questionnaires and data collection procedure by the main investigator. Pre-test in 10% of the sample size was done in Boru hospital which was not included in the actual study. The respondents encouraged to respond to all items in the questionnaire within the time they devoted.
Operational definitions
• Good knowledge: Health workers who answered ≥ 70% of knowledge questions correctly.
• Poor knowledge: Health workers who answered < 70% of knowledge questions correctly.
• Favorable attitude: Health workers who answered ≥ 70% of attitude questions.
• Unfavorable attitude: Health workers who answered < 70% of attitude questions.
• Good practice: Health workers who have properly practiced ≥ 70% of practice questions.
• Poor practice: Health workers who have practiced < 70% of practice questions.
Data analysis
The data was entered, cleaned and analyzed by using SPSS version 20 software and described by using tables and graph.
Ethical consideration
Ethical clearance was obtained from Wollo University, college of medicine and health sciences, department of comprehensive nursing research committee. Official letter from department of nursing was written to DRH. Written consent was obtained from all study participants after information is provided about purpose of the study and confidentiality of the information.
Socio-demographic characteristics of the study participants
Out of the total sample size (n = 211), 191 study subjects were participated in the study which gives a response rate of 90.5%. The mean age of the study subjects was 29.87 years (+ 6.76 SD). One hundred fifteen (60.2%) of respondents were males and the rest 76 (39.8%) were females (Table 1).
| Table 1: Sociodemographic characteristic of health workers at Dessie referral hospital, North East Ethiopia. | |||
| Variables | Frequency (n = 191) | % | |
| Age | 19 - 28 | 117 | 61.3% |
| 29 - 38 | 59 | 30.9% | |
| 39 - 47 | 9 | 4.7% | |
| > 47 | 6 | 3.1% | |
| Sex | M | 115 | 60.2% |
| F | 76 | 39.8% | |
| Educational status | Diploma | 69 | 36.1% |
| Degree | 96 | 50.3% | |
| Above | 26 | 13.6% | |
| Level of experience | ≥ 5 years | 151 | 79.1% |
| 6 - 10 years | 23 | 12% | |
| ≥ 11years | 17 | 8.9% | |
| Profession | Nurse | 100 | 52.4% |
| Medical laboratory | 13 | 6.8% | |
| Pharmacy | 18 | 9.4% | |
| Doctor | 25 | 13.1% | |
| Anaesthetists | 3 | 1.6% | |
| Psychiatry | 3 | 1.6% | |
| Ophthalmology | 3 | 1.6% | |
| Midwives | 18 | 9.4% | |
| Radiology | 5 | 2.6% | |
| IESO | 1 | 0.5% | |
| Dentist | 1 | 0.5% | |
| Physiotherapy | 1 | 0.5% | |
Health care workers knowledge towards hospital acquired infection prevention
Overall 165 (86.4%) health workers had good knowledge and the rest 26 (13.6%) of respondents had poor knowledge towards HAIPs. Even though most of the respondents had good level of knowledge regarding HAIPs, a significant number of respondents had misconception about HAI includes Ventilator associated pneumonia (VAP), Tuberculosis (TB), UTI, gastroenteritis (30.4%) and patient history will influence decision in choosing personal protective equipment (PPE) (44.5%) (Table 2).
| Table 2: Health care workers knowledge towards hospital acquired infection prevention at DRH, Ethiopia. | |||
| Characteristics | Frequency (n = 191) | % | |
| Nosocomial infection is an infection whose development is favoured by a hospital environment | true | 186 | 97.4% |
| false | 5 | 2.6% | |
| Nosocomial infections includes Ventilator associated pneumonia(VAP),Tuberculosis, Urinary tract infection, Gastroenteritis | true | 133 | 69.6% |
| false | 58 | 30.4% | |
| Hepatitis B virus, Hepatitis C virus, Staphylococcus aureus and Pseudomonas aeruginosa are the organisms commonly encountered in nosocomial infections | true | 172 | 90% |
| false | 19 | 10% | |
| Gloves should always be worn in contact precautions | true | 160 | 93.8% |
| false | 31 | 16.3% | |
| Standard precautions should include the use of protective equipment and frequent hand washing | true | 175 | 91.6% |
| false | 16 | 8.4% | |
| Diagnosis influences my decision in choosing Personal protective equipment (PPE) | true | 136 | 71.2% |
| false | 55 | 28.8% | |
| Patient history will influence my decision in choosing PPE | true | 106 | 55.5% |
| false | 85 | 44.5% | |
| Washing hands before and after handling patients helps to prevent infection | true | 178 | 93.2% |
| false | 13 | 6.8% | |
| Wearing N95 mask is important when dealing with air born infection | true | 169 | 88.5% |
| false | 22 | 11.5% | |
| Wearing surgical masks when doing surgical procedures is vital to prevent infection | true | 186 | 97.4% |
| false | 5 | 2.6% | |
Health care workers attitude towards hospital acquired infection prevention
In general the result indicates that 146 (76.4%) had favorable attitude while 45 (23.6%) had unfavorable attitude towards HAIP activities. Significant number of respondents didn`t agree in the importance of changing mask before going to another patient as a nosocomial infection control measure (disagree + not sure = 37.2%) (Table 3).
| Table 3: Health care workers attitude towards hospital acquired infection prevention at DRH, Ethiopia. | |||
| Characteristics | Frequency (n = 191) | % | |
| Categorize hospital waste | Agree | 1183 | 95.8% |
| Disagree | 6 | 3.1% | |
| I am not sure | 2 | 1.1% | |
| Hand hygiene after removing gloves | Agree | 174 | 91.1% |
| Disagree | 14 | 7.3% | |
| I am not sure | 3 | 1.6% | |
| Skin disinfection is necessary to prevent nosocomial infection | Agree | 153 | 80.1% |
| Disagree | 31 | 16.2% | |
| I am not sure | 7 | 3.7% | |
| Invasive procedures are not risk factor for multi-drug resistance organisms | Agree | 59 | 31% |
| Disagree | 119 | 62.3% | |
| I am not sure | 13 | 6.7% | |
| Health worker hands are vehicle for transmission of nosocomial pathogen | Agree | 146 | 76.4% |
| Disagree | 36 | 18.8% | |
| I am not sure | 9 | 4.8% | |
| Changing mask before going to another patient | Agree | 120 | 62.8% |
| Disagree | 65 | 34% | |
| I am not sure | 6 | 3.2% | |
Health care workers practice towards hospital acquired infection prevention
Overall the result showed that majority of respondents had poor practice 147 (77%) and 44 (23%) of them had good practice towards HAIP activities. Only 56 (29.3%) always wash hands before start work (Table 4).
| Table 4: Health care workers practice towards hospital acquired infection prevention at DRH, Ethiopia. | |||
| Characteristics | Frequency (n = 191) | % | |
| Wash hands before start work | Always | 56 | 29.3% |
| Often | 50 | 26.2% | |
| sometimes | 80 | 41.9% | |
| Not at all | 5 | 2.6% | |
| Wash hands before handle new patients | Always | 48 | 25.1% |
| Often | 72 | 37.7% | |
| sometimes | 60 | 31.4% | |
| Not at all | 11 | 5.8% | |
| Change gloves before handling new patient | Always | 61 | 31.9% |
| Often | 97 | 50.8% | |
| sometimes | 32 | 16.8% | |
| Not at all | 1 | 0.5% | |
| Wear mask when handling TB suspected patients | Always | 67 | 35.1% |
| Often | 67 | 35.1% | |
| sometimes | 51 | 26.7% | |
| Not at all | 6 | 3.1% | |
| Taste samples using safety cabinets | Always | 46 | 24.1% |
| Often | 71 | 37.1% | |
| sometimes | 63 | 33% | |
| Not at all | 11 | 5.8% | |
| Discard infectious materials and left over samples according to the guide line | Always | 31 | 16.2% |
| Often | 84 | 44% | |
| sometimes | 73 | 38.2% | |
| Not at all | 3 | 1.8% | |
In this study 86.4% of health workers had good knowledge which was in line with the study conducted in Bahirdar city, Gondar and Debre Markos referral hospital which were reported as 84.2%, 81.6% and 84.7% of health workers had good knowledge respectively [11-13]. On the other hand this finding is relatively lower than similar study conducted in Egypt, Cairo university hospital which reported as 90% of respondents had good knowledge [14]. In the current study 93.8% of respondents were knowledgeable as gloves should always be worn in contact precaution which is higher than a study conducted in Mizan Aman general hospital which was reported as 70.4% of respondents knew this [15]. This difference might be attributed to the difference in the academic background of the study respondents, setting of the study, sampling technique, sample size between studies and infection prevention guideline availability. More than two third (76.4%) of the respondents had favourable attitude about HAIP which was higher than similar study conducted in Bahirdar city 55.6% [11] and Gondar (64.2%) [12]. The possible explanation for difference might be due to difference in methodology, work experience, educational level, training opportunity, and personal characteristics of the study participants between various studies.
Less than one fourth (23%) of HCW had good practice towards HAIP. This showed that presence of main concern in HCW practice regarding to HAIP that needs immediate attention. This finding was much lower than similar studies conducted in different areas like Bahirdar city (54.2%), Gondar university referral hospital (57.4%) and Debre Markos (57.3%) and Mekele (42.9%) [11-13,16]. This lower result might be due to scarcity in availability of sanitary facilities and logistics required for HAIP activities at the current study site. Our study showed that 25.1% of respondents wash their hand before handling new patients which extremely lower than similar studies conducted in Mizan Aman general hospital and Saudi Arabia reported as 68.7% of study subjects and 88.5% nurses and 68% doctors wash their hands always before handling new patients respectively [15,17] but higher than a study conducted in Cairo University, Egypt and Addis Ababa Ethiopia reported only 15% and 7% of respondents wash their hands before handling new patients respectively [14,18]. The reason for this difference might be explained by the differences in logistics and facilities required for prevention of HAI in the study areas. In this study 31.9% of respondents always change gloves before handling new patients. This result was lower than the study conducted in Italy in which 87% always change gloves [19]. The reason for this poor practice might be due to inaccessibility of gloves in each outpatient department, ward and laboratory rooms in the present study. In the current study only 16.2% of respondents always discard infectious materials and left over samples according to the guide line. This showed that presence of huge gap concerning to infection prevention of the hospital.
Overall this study result indicates poor practice towards HAIP so that the health system and the policy makers should put their effort in order to improve quality of health care with regard to infection prevention. Even if the majority of health care provider had good knowledge and favourable attitude towards HAIP, still it needs improvement. Therefore the health system and the policy makers should do to increase KAP of the health care workers towards HAIP so that the community will be benefited.
Most of respondents had good knowledge and considerable high level of favorable attitude but majority of respondents had poor practice i.e. they do not always wear masks and gloves, wash hands and they do not discard infectious materials according to the recommendations of the guideline. Therefore Dessie referral hospital health workers should strictly follow HAIP guideline and the hospital administrators should fulfil necessary supplies for infection prevention. Researchers should also do further study by using mixed qualitative and quantitative methods to address the unreached problems of the hospital.
Implications for clinical practice
The health care workers play significant role in preventing infection among the hospital patients and themselves. The finding of this study alerts health workers to follow the infection prevention guide line to prevent infection and consequently enhance the quality of hospital care. Regarding research, the study findings also provide basis for other researchers who would want to carry out further research on infection prevention and control principles.
Authors would like to acknowledge Dessie referral hospital and the study participants who provided valuable information with their full cooperation. We also acknowledge the data collectors and supervisor for their time and full commitment.
- Allegranzi B, Nejad SB, Combescure C, Graafmans W, Attar H, et al. Burden of endemic health-care-associated infection in developing countries: systematic review and meta-analysis. The Lancet. 2011; 377: 228-241. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/21146207
- Infection control and quality; 13 most common health care associated infections. 2014.
- Mortell M, Balkhy HH, Tannous EB, Jong MT. Physician ‘defiance’towards hand hygiene compliance: Is there a theory–practice–ethics gap? J Saudi Heart Assoc. 2013; 25: 203-208. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/24174860
- Abdallah SA, Al-Shatti L, Al-Awadi B, Al-Hammad N. Disinfectants use awareness among college of nursing students and nurses in some healthcare settings, Kuwait. Middle-East Journal of Scientific Research. 2012; 12: 964-969.
- Mortell M. Hand hygiene compliance: is there a theory-practice-ethics gap? Br J Nurs. 2012; 21: 1011-1014. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/23123746
- Al-Jubouri MBAJ. Assessment of Nurse's Knowledge about Nosocomial Infection at Hospitals in Baghdad City. Kufa Journal for nursing sciences. 2014; 4: 198-203.
- Federal Ministry of Health. Infection prevention and patient safety reference manual for health providers and managers in health care facilities 2010: 92-93.
- Reda AA, Fisseha S, Mengistie B, Vandeweerd JM. Standard precautions: occupational exposure and behavior of health care workers in Ethiopia. PLoS One. 2010; 5: 14420. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/21203449
- Mehta Y, Gupta A, Todi S, Myatra S, Samaddar D, et al. Guidelines for prevention of hospital acquired infections. Indian J Crit Care Med. 2014; 18: 149. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/24701065
- Suchitra J, Devi NL. Impact of education on knowledge, attitudes and practices among various categories of health care workers on nosocomial infections. Indian J Med Microbiol. 2007; 25: 181. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/17901633
- Gulilat K, Tiruneh G. Assessment of knowledge, attitude and practice of health care workers on infection prevention in health institution Bahir Dar city administration. Sci J Public Health. 2014; 2: 384-393.
- Yazie TD, Sharew GB, Abebe W. Knowledge, attitude, and practice of healthcare professionals regarding infection prevention at Gondar University referral hospital, northwest Ethiopia: a cross-sectional study. BMC research notes. 2019; 12: 1-7. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/31500659
- Desta M, Ayenew T, Sitotaw N, Tegegne N, Dires M, et al. Knowledge, practice and associated factors of infection prevention among healthcare workers in Debre Markos referral hospital, Northwest Ethiopia. BMC health services research. 2018; 18: 465. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/29914477
- El-Sayed M, Gomaa M, Abdel Aziz M. Nurses’ knowledge and practice for prevention of infection in burn unit at a university hospital: suggested nursing guidelines. J Nurs Health Sci. 2015; 4: 62-69.
- Yakob E, Lamaro T, Henok A. Knowledge, attitude and practice towards infection control measures among Mizan-Aman general hospital workers, South West Ethiopia. J Community Med Health Educ. 2015; 5: 1-8.
- Gebresilassie A, Kumei A, Yemane D. Standard precautions practice among health care workers in public health facilities of Mekelle special zone, Northern Ethiopia. J Community Med Health Educ. 2014; 4: 286.
- AL-Saleh EM, Ibrahim A, Lillian M. Healthcare workers’ knowledge, attitudes and practices in King Fahad Hofuf hospital, Saudi Arabia. Journal of pharmaceutical and biomedical sciences. 2014; 4: 410-421.
- Tenna A, Stenehjem EA, Margoles L, Kacha E, Blumberg HM, et al. Infection control knowledge, attitudes, and practices among healthcare workers in Addis Ababa, Ethiopia. Infect Control Hosp Epidemiol. 2013; 34: 1289-1296. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/24225614
- Parmeggiani C, Abbate R, Marinelli P, Angelillo IF. Healthcare workers and health care-associated infections: knowledge, attitudes, and behavior in emergency departments in Italy. BMC infectious diseases. 2010; 10: 35. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/20178573